This essay was submitted to Open Philanthropy's Cause Exploration Prizes contest.
If you're seeing this in summer 2022, we'll be posting many submissions in a short period. If you want to stop seeing them so often, apply a filter for the appropriate tag!
1. Introduction
For to everyone who has will more be given, and he will have abundance; but from him who has not, even what he has will be taken way.
- Matthew 25:29, RSV
It is also true when it comes to healthcare inequalities for children. Children is the hope for the future of human race. Per advised by the WHO/UNICEF Nurturing care framework, it takes 5 main factors to ensure the healthy growth of children: health, nutrition, responsive care giving, secure-safe environment and early education opportunity. While education inequality is often noticed, the disparity of pediatrician access is neglected. Pediatrician is directly related to ensure the health and nutrition of the children. The shortage of pediatrician, however, is increasingly severe in LMIC countries, especially in Africa and South-East Asia.
In this paper, I will argue why pediatrician is essential to the healthy growth of children. I will then discuss the social-economic reasons and personal reasons causing the shortage of pediatrician. Without social interventions, shortage of pediatrician will always exist and become insufficient in areas or countries with low economic level. I will then describe in what ways the funding can improve the situation, and what are the metrics to track the success of the programs.
2. Existing problems description (what is the problem)
2.1 Pediatrician density
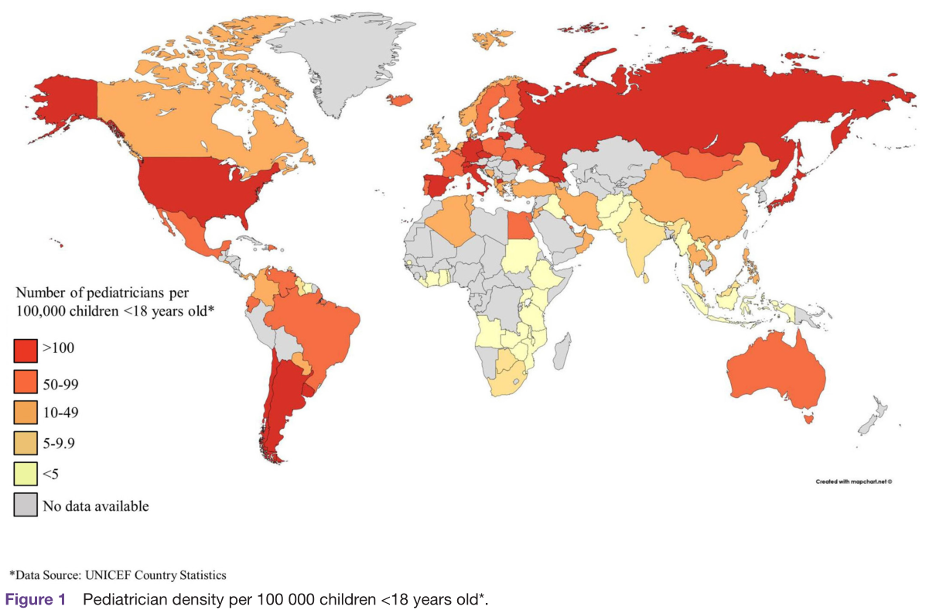
Pediatrician density (measured as number of pediatricians per 100,000 children) is a metric to track the supply of pediatrician in a specific region.
According to existing research, pediatrician density varied significantly by GDP[1], ranging from a median of 0.5 pediatricians per 100,000 children in low-income countries to a median of 72 pediatricians per 100,000 children in high-income countries. The global median density rate is 32 pediatricians per 100,000 children. Among the countries, the lowest density rate was found in Africa (0.8) and South-East Asia (4)[2]
What’s even worse is that fewer pediatricians are entering the workforce, which might exacerbate the already existing disparities of pediatrician distribution. The number of incoming pediatricians entering the workforce is also varied by economic levels. In low-income countries, there is a median 10 new pediatrician entering the workforce (or 0.08 per 100,000 children). In Africa, this number is 5 new pediatrician (0.08 per 100,000 children) per year compared to global average of 30 (1.44 pediatrician per 100,000 children)[3].
The deficiency in supply of pediatricians will increase the workload of working pediatricians, and thus further increase the turnover rate. Less pediatricians willing to enter the workforce and less willing to remain are two key factors that contribute to the total shortage in pediatricians. This problem is especially severe in Africa and Southeast Asia, the areas which bear the highest disease burdens. Over half of the world’s 5.4 million under-five death in 2017 occurred in Africa[4]. If leaving unattended, large percentage of newborns and young children will not be covered by health professionals.
Picture 1[5]
2.2 How many people are impacted?
Though all countries suffered from shortage of pediatricians, but the children in South-east Asia and Africa have the lowest pediatrician density. Children in South-East Asia amounted to 627 million children under 18 years old[6]. For Africa this number is 650 million[7]. Africa is on its way to become the continent having the largest child population. A total of 1,277 million children (under 18 years old) are impacted. The total world population is about 7,875 million as of July, 2021[8]. In conclusion, a total of 16% world population is impacted.
3. Why are pediatricians important? Why is shortage causing harms?
As defined by American academy of pediatrics, a pediatrician is a physician who is concerned primarily with the health, welfare, and development of children, and is uniquely qualified for these endeavors by virtue of interest and initial training[9]. A pediatrician covers a person from its birth to young adulthood. The definition of early adulthood varies by country as 18 years old or 14 years old. The pediatrician is essential to the healthy development of child, especially in early child development (defined age between 0 – 7 years old).
As pointed out by the WHO/UNICEF Nurturing care framework, 5 main factors determine the success of early childhood development: that is health, nutrition, responsive care giving, secure-safe environment and early education opportunity[10]. Nutrition is directly linked with health and disease, morbidity and even mortality of children. A pediatrician is directly involved in health and nutrition of children and could also detect early signs should any wrong doings happened in private family lives such as physical abusing, sexual harassment, or misconduct in caregiving. Though not directly involved, Pediatrician can act as a third-party guardian linked to secure-safe environment from a society’s perspective.
In other words, shortage of pediatrician will leave the newborns and children unattended by healthcare workforce, and will lack care in health and nutrition, and preventive care in diseases that causing early deaths. Moreover, it also exposes children to potential safe issues at homes or neighborhoods without being detected by society.
4. What is potentially causing the shortage in pediatrician in LMIC countries?
I want to find out what is causing shortage in pediatrician in certain regions. From the existing research done on disparities of pediatrician access globally, there are social economic reasons and personal reasons causing shortage of pediatrician. The social economic reason in turn fuels the personal reason, which further increases the disparity of access to pediatrician.
4.1. Social-economic reasons causing the disparity of pediatrician distribution
For social economic reasons, the research found statistically significant positive correlation between per capita income and access to pediatric care[11]. In research on disparities of access to pediatric care in Poland, results present that there is a significant (0.686, p=0.004) correlation between accessibility to pediatric care with disposable income[12]. It means for cities which have higher per capital income, or simply cities which are wealthier, they have more numbers of pediatrician and can thus offer more pediatric care to children. The research also identified the pediatric workload, measured by TPP (number of patients per pediatrician) was negatively correlated with the availability of public pediatric service accessibility[13]. And the correlation is of statistical significance (-0.618, p=0.005). Lack of pediatrician will increase the workload of the existing pediatrician already working in the specific region, and this over-workload will lead to more pediatrician leaving the field or transition to adult healthcare. We will see the workload burden as one of the main reasons for high pediatrician turnover in following analysis. In conclusion, the unevenly distribution of disparities is due to social-economic reasons. Furthermore, such disparity in turn increases the workload for the already scarce pediatrician workforce. The vicious cycle is thus completed.
4.2 Lack of qualified training resources
There are more resources concentrated in provinces or countries with higher level of social-economic development[14]. Hospitals are closely connected to medical schools and universities for research purposes. The latter supplies doctors whether its general practitioners or specialized doctors or pediatrician. For a graduated pediatrician, it is more likely for him/her to choose to work in an area close to the schools.
Another reason might be the existence of training capacity gap[15], there are fewer avenues to train pediatricians or fewer opportunities for employment in LMIC countries. In China, for example, there is a lack of educational resources for training pediatricians. 32% of pediatricians had only completed 3 years of junior college or polytechnic school education after high school[16].
In Sub-Sahara for example, the lack of quality training is due to a. decaying infrastructure and inadequate funding, b. lack of faculties, c. increasing number of students unmatched by available teaching and training facilities and resources[17]. As a result, small number of graduates, and high emigration to developed countries, both contribute to low physician presence in Africa[18].
Moreover, to go to medical school is a huge investment in both time and money. I checked online information on how long it takes to pursue a career in pediatrician. It generally takes about 11 years for completion[19]. Firstly, you need to complete bachelor’s degree which takes 4 years, then 4 years of medical schools, and 3-5 years of residency programs. I checked online for the tuition. The medical school 4 years in U.S. and Canada cost roughly $240,000 ($60,000 per year for non-residency). The medical schools in South Africa cost cheaper. $20,000 for 4 years ($5,000 average per year). This amount of invested time and money can be daunting to majority from local humble families.
4.3. Personal reasons: burnouts, huge pressure, and low compensation
All are reasons to cause existing pediatrician transition to other fields, or current medical students unwilling to pursue pediatrician track.
4.3.a Job Burnouts
Due to the high workload, large percentage of pediatricians will suffer from certain level of burnouts. This work fatigue is especially common in LMIC countries, where the presence of qualified pediatrician is scarce. I took reference of a report done on burnout of pediatrician in Guangzhou, China. China has a pediatrician density of 40 pediatrician per 100,000 children[20]. Of the 370 surveyed pediatrician working in Guangzhou municipal hospitals, 272 pediatricians (73.51%) showed different degrees of job burnout. 117 pediatricians (31.62%) showed moderate burnout[21]. This burnout ratio is higher than other specialty surveyed.
Among the burnout reasons, emotional exhaustion scored the highest, this might be due to the pediatrics nature: to interact with children and their parents with high expectations.
Another burnout reason is low level of social support. In the survey 61.35% of pediatrics reported low level of social support. Among various perspectives of social support, objective social support scored the lowest (38.55%)[22]. Objective social support means material compensation and actual support received from colleagues and social network. Pediatricians have nobody to turn to when they meet personal finance issues or workload issues. Additionally, pediatricians are also paid the least among all the specialties (discussed in the 4.3.c).
4.3.b Increased tension between patient’s family members and pediatrician
Children, unlike adults, are usually accompanied by parents to visit a pediatrician. When communicating with pediatrician, they are not as clear as adults to articulate the symptoms and describe the illness. Therefore, they often rely on parents when seeking diagnosis from pediatrician. Parents, however, are usually very protective of their children, especially when it concerns the health of children. In China and eastern cultures, parents often have high expectation on their offspring. They transferred such high expectation to pediatrician. Some parents have unrealistic expectation for pediatrician. Once the pediatrician fails to meet such high expectation, parents will often exuberate unreasonable emotions, often in threatening acts or behave aggressively to the pediatrician[23]. Back in 2006 the Pediatric Society of Chinese Medical Doctors Association reported 831 incidents of medical violence towards pediatrician, among which 319 attacks have beaten the medical workers or pediatrician involved to death or disabled. Up till now the medical violence still appears in news from time to time.
This makes the pediatrics job not only burdensome but also dangerous. When a pediatrician sees a child, he/she also needs to bear the pressure coming from the child’s parents. And the potential aggressive behaviors towards the pediatrician, is one of the main sources of pressures[24].
4.3.c Low pay while high workload
Even in U.S., pediatrician is the lowest paid medical jobs. I found in a 2015 physician compensation report that surveyed more than 19,500 doctors across 25 specialties, pediatricians were paid the least with an average yearly salary of $189,000, that is 3% less than the family medicine doctor, 13% less than the psychiatrists, 17% less than neurologists, and 40% less than general surgeons.
Table 1[25].
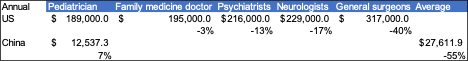
This low pay condition is even more severe in LMIC countries. Take China for example, China is known for its vast population and is also under the shortage of pediatricians. In China majority of medical resources are concentrated in public hospitals. I searched online for average salary of pediatrician in China. The average pediatrician in China has a salary of $12,537, only 7% of average pediatrician salary in U.S. Compared to average medical doctors’ salary of $27,611, pediatrician salary is 55% less than the average.
For medical students who pursue the pediatrics track, they spend the same amount of investment in medical school and residency programs, and yet they are paid the least among all medical specialties. Additionally, they are more likely to get job burnouts and find less social support whenever they need. All these factors make pediatrics a low value-for-investment choices from career choosing perspective. It is fair to conclude that people make economic choices when it comes to choosing a career. Without social interventions less students will choose pediatrics or potentially leave pediatrics and transition to other specialties.
From a China national survey on work plans of pediatricians, 34% of the pediatricians have resignation plans within the next 2 years. 23% is not sure and still hesitating. Over 41% of the pediatricians based in the primary hospitals in rural areas are thinking about resignation in the next 2 years[26]. China’s current strategy is to lower the barriers for pediatricians entering the workforce, however, this does not solve the problem of the retention rate and might even lower the workforce quality.
5. What is the nonprofit addressing this problem? Is any funding directed to this?
5.1. Community Pediatrics Training Initiative, U.S.
I found an initiative in U.S. called Community Pediatrics Training Initiative founded by famous pediatrician Anne Dyson. The program is aimed to establish pediatric residency training programs that would train pediatricians who have greater skills and interest in community-based medicine, advocacy, and who are better able to improve the health of children in their communities[27]. A total of 10 pediatric departments throughout the U.S. received the grants (5-year grant ranging from $1.7M to $2.5M). The program will host classroom training, online training, case study, essay reading and attending conference, to enhance the qualities of community pediatrics.
The program is hosted by Anne Dyson’s family foundation – Dyson Foundation.
5.2. the African pediatric fellowship program (APFP), Africa
This program provided residency training to post-graduates pursuing pediatricians and trainees interested in child nurses. It aimed to train trainees beyond South Africa (where current medical resources is clustered) and encourage the graduated trainees to return to their home country for leading the pediatrics force. The APFP program has partnerships with 40 medical institutions across 13 countries in Africa[28]. So far it has trained 236 child-health specialists from 17 countries across Africa. More than 90% have returned to their home countries. Upon returned to their home countries, the trainees are using the expertise and knowledge learnt to train local doctors and nurses. Moreover, the program also created a supportive alumni network connecting pediatricians and related professionals across Africa, providing a platform for knowledge sharing and best practices[29].
The surprising high return of the trainees is contributed by the program design. The participating medical institution identifies an area of need and nominates a potential trainee who is guaranteed a position on return upon completion of the program[30]. It provides trainees more incentive for return if they know they could secure a leadership position in the specific area in local hospitals. After returned, the trainees resume the core force in building academic departments, and conducting medical research, and leading the evolution of the local pediatrics sector.
Trainee to trainer ratio is kept at 2 fellows to 1 attending physician to ensure the program quality. For curriculum design, the program combined clinical rotations with protected time for research. The trainees are provided chances to present at national or international conferences. Some have received awards and grant funding. What makes the program so tailored to the local community is that the training program is structured to the needs of the fellow’s home institution instead of a general practice and advantages of the host country. The trainees are more likely to return because they know for sure their expertise can directly help the local community. The design of the program provides a good guidance should OP like to develop a related nonprofit project.
The funding of the APFP program is supported by international philanthropic and nongovernment organizations, as well as funding from referral hosting institutions[31]. Take their pediatric pulmonology program for example, a single fellow costs $25500 a year. Funding for two-year program is $50,000 per fellow. Graph 2[32]
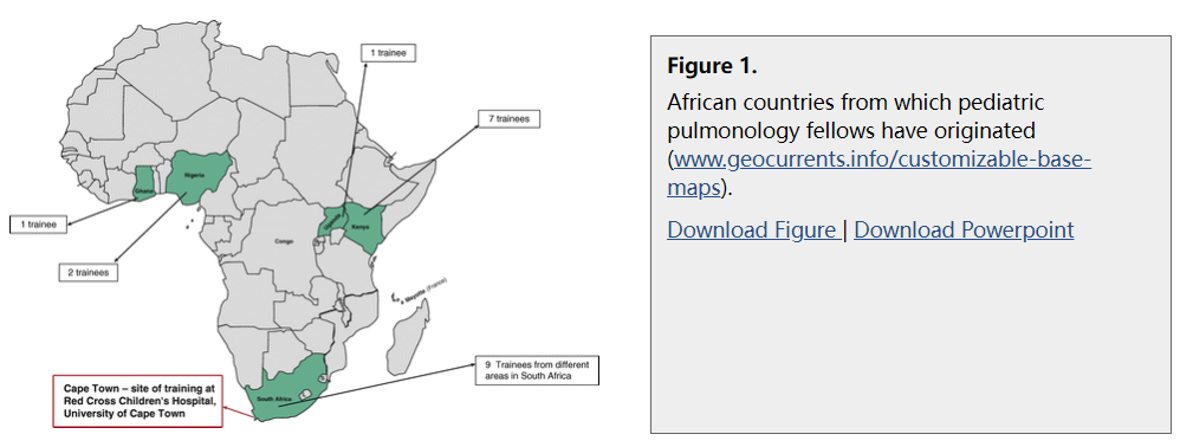
The funding NGOs and non-profits include: the Children’s Hospital Foundation, Red Cross War Memorial Children’s Hospital, Harry Crossley Foundation, ELMA Foundation, Vitol Charitable Foundation, Cadbury Foundation, Mauerberger Foundation, Phatisa Foundation, German Academic Exchange Service (DAAD), the University of Cape Town, and the referring African institutions[33].
6. How should the investment help this? How should the program be carried out?
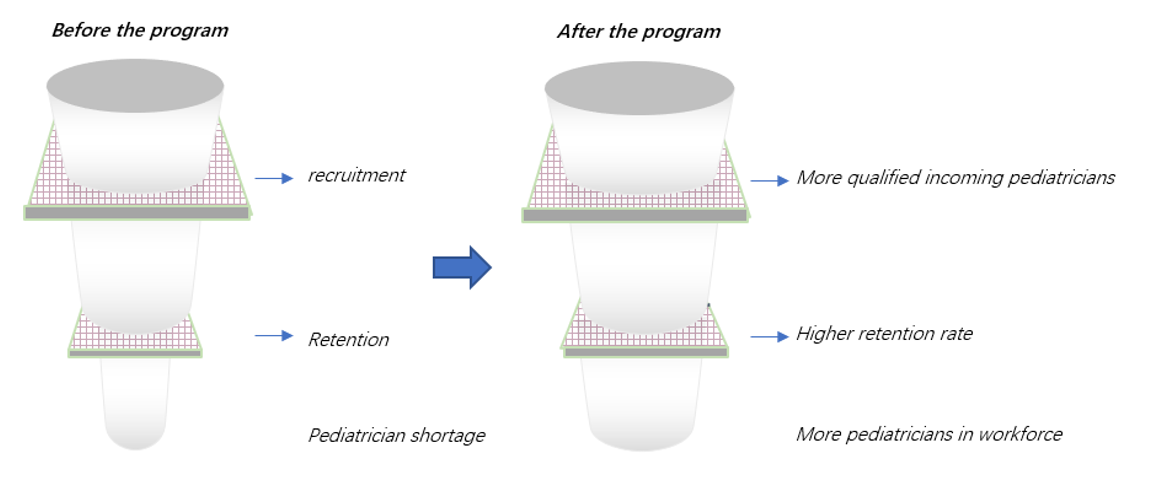
I have explored the below solutions for the potential programs carried out to reduce the shortage of pediatricians in LMIC countries. I think the program can try to solve two critical problems: 1. Increase supply of pediatrician in LMIC countries where medical education resource is scarce, 2. Increase the retention of pediatrician in the workforce. There are several ways for funding opportunities:
6.1 The program can fund the training of the pediatrician workforce in LMIC countries, starting with 1 or 2 target countries and evaluate the results first.
The OP will find 5 medical schools in U.S. to partner with 2-3 local medical schools in LMIC, to create a 2+2 year program. This program will specifically recruit (say 30) local students committed to take the pediatrician track. They will spend 2 years studying in local medical schools, and then 2 years in the partnered medical schools in U.S. When it comes to choose residency, the students of this program MUST follow the pediatrics track. For the residency students will spend 1 year in top U.S. hospitals pediatrics department, and then 2 years back in their own country. The fund will cover the expenses for students (including tuition) for the 3 years in U.S. (2 years study and 1 year in residency) including the tuition and expected living expenses.
In U.S. medical training systems, the education in bachelor’s degree and medical school 1st and 2nd years are same for students choosing different specialties. In 3rd year and 4th years, students can choose area of focus and then intern at hospitals (or residency programs) in specialty. This funding program is designed to attract and provide education access to LMIC students who want to take pediatrics specialty.
But note pediatrician workforce is even in shortage in some developed countries such as UK. There could be a brain drain problem, where the pediatricians will stay in areas of higher economic levels. In the UK workforce consensus report, it specially asked the policy makers to attract more overseas-trained doctors and health professionals to compensate the local shortage[34]. In USA and UK, it is estimated one third of the pediatrician workforce are international medical graduates[35]. So further questions for this program is how to encourage the funded students to return to their own countries after they have trained and worked in residency in U.S.
6.2 Rotation residential programs
Another more economics way is to fund the residency programs directly. This program can target post-graduate medical students, those who have already finished academic studies. Like African pediatric fellowship program, this program can create rotational residential opportunities between host institutions and participating institutions. The rotational can be both ways, the experienced physicians in the host institutions, often better pediatric hospitals, can work and help to train local residency trainees. Or the local trainees can come to finish the residential years in hosting institutions.
The funding will be given to experienced pediatricians or local trainees during their rotational program, including transportation expenses, housing and stipend. Part of the fund will also go to the program operations. The host institutions will make the budgets for OP’s detailed review – including salary for the trainees, the cost for hosting seminars, research opportunities, etc.
For participating institution, they need to have a detailed plan of the positions and detailed job responsibilities for the trainee upon return. They should also articulate how they want the program to help them and identify a pediatric area of focus they want the trainee to focus on.
6.3 Promote primary care in pediatrics to share responsibilities and promote preventive care
This might seem common in developed countries, for many LMIC countries lacking in medical resources, patients like to swarm to hospitals when they spot some illness. And this creates huge burden for both patients and doctors. In an analysis of a third-grade class-A hospital in Beijing, 60% of the pediatric cases are common diseases and can be cured in primary care[36]. Community pediatrics, if followed by right trainings, should be able to cure these and refer the remaining to specialty care if needed. The tertiary referral structure is very mature in U.S., but still nascent in LMIC countries.
Good community pediatrics can also provide good preventive care to children, therefore reduce the ultimate number of patients visiting specialty pediatricians. LMIC countries tend to have lower regular primary care rate (64% response rate in LMIC than 91% worldwide)[37]. The primary care can offer preventative and promotive care throughout childhood including but not limited to health checks, nutrition assessment, growth monitoring, immunization, and vaccination etc.
6.4 Increase health workforce facilitating pediatrics: i.e., children’s nurses, health visitor, etc.
In the job burnout section, we have discussed one of the main reasons for job burnout is lack of objective social support. Grants can be used to implement training programs for health workforce who can share the responsibility. Some of the procedural work can be done by children’s nurses, or health visitors or primary care (mentioned in 6.3).
Increase Health care staff facilitating pediatrician can alleviate the latter’s work burden. In Switzerland and U.S. for example, family doctors take care of roughly 20% of the child health workload[38]. When it comes to lower individual burden, It is necessary to build a child health force and outsource some of the pediatrician work to the team instead of relying solely on pediatrician himself/herself. The child health force also includes children’s nurses, health visitors, mental health professionals, primary care, and allied health professionals[39].
7. Metrics and tractability
7.1 Access to pediatrics: pediatrician density ratio - # of pediatrician per 100,000 children
This ratio measures the access to pediatrician for each area or country. Measured by number of pediatricians per 100,000 children, children here are defined as people under 18 years old. Depends on the varied health system, in some countries children transition to adult care at the age of 18 or earlier in age 14. So, the children number will be adjusted according to the specific definition. The tracking of this ratio can evaluate if the disparities of pediatric distribution has been gradually improved.
7.2 Number of visits per pediatrician per day (including outpatient, inpatient and emergency visits)
This ratio can be used to effectively measure the workload of pediatrician. The decrease of this ratio can suggest the burden of pediatrician is shared by healthcare workforce, contributing by more incoming pediatricians, or addition of trained pediatric health workers (including community pediatrics, child nurse etc.)
An increase ratio also suggests that the pediatrician is experiencing heavier work burden, an implication in lack of peer pediatricians, or other pediatric workforce that can assist the process. This should be alarming and might eventually lead to work burnout and turnover.
This ratio can be also horizontally compared to doctors of adult care or across tiers of hospitals to imply the work burden carried by pediatrician. A further analysis on the workload is also available by dissecting the formulas:
Outpatient care = pediatric outpatient visits/pediatrician year[40]
Inpatient = pediatric beds * turnover rate/pediatrician/year[41]
7.3 Retention rate (or turnover rate): 1 year retention rate (and 3,5 years rate)
Retention rate measures the remain of pediatricians. Ideally, we would like to see a gradual increase of retention rate, implying the work burden is bearable contributed by more pediatric workforce, and the work condition has been improved. A decrease in retention rate calls alarm to investigate the reasons of dropping out. Increasing drop out of pediatricians will exacerbate the shortage of pediatricians.
A detailed analysis on the drop out rate (measured as 1 – retention rate) is also available. There are usually two exit ways of pediatrician: 1. Leave the pediatrics field and transition to adult care or other medical specialties, 2. Leve the medical area completely and go for other industry). Further analysis can be done in analyzing transition rate, to see percentage of pediatrician transition to adult care or other specialties.
The program to reduce the shortage in pediatrics should ideally see an improvement of the above-mentioned ratios in the long term: increase the pediatrics density ratio and decrease the number of visits per pediatricians per day to a healthy level, and eventually increase the retention rate. Other Long-term metrics include positive impacts on U5MR (under 5 mortality rate). This ratio includes comprehensive factors from social and economic development, might be too macro to track the pediatrics contribution.
Graph 3
8. Other questions to consider
8.1 Region specific conditions
The reasons of shortage in pediatric diseases vary by country. Further research in specific country: including medical school resources, common diseases, local hospital resources etc. need to be in place before conducting the funding.
There also exists region specific diseases when it comes pediatric specialty. For example, pneumonia, malaria and diarrhea accounted for 36% of under five deaths in Africa[42]. To make the program more efficient, it is worthwhile to investigate the region-specific diseases leading to causes of death. The pediatricians can be trained in specialty according to the local needs and urgency.
8.2 Brain drains or pediatric migration to high income countries - how to encourage the funded trainees to return to their home country and improve the local pediatrics.
8.3 We want the individual trained pediatricians to create bigger impacts.
While our funding can directly impact individual pediatricians, we should also think about how to make the individual make bigger impacts and lead the transformation of local pediatrics. For example, the pediatricians can influence local policy makers, are given the resources from authority to lead own research, help to form the training for incoming pediatricians, etc.
Citings:
Note: there are several citings on different sections of one paper
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
Unicef, Children in Africa, key statistics on child survival and population
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
- ^
- ^
UN (world population prospects 2019), Oct 2021
- ^
E. Ozmert, Early childhood development - the role of pediatrician, 2021
- ^
2018 WHO/UNICEF nurturing care framework, World Health Organization 2018
- ^
T.Zienkiewwicz, M. Klata et al, Determinants and disparities in access to pediatricians in Poland, April 2022
- ^
T.Zienkiewwicz, M. Klata et al, Determinants and disparities in access to pediatricians in Poland, April 2022
- ^
T.Zienkiewwicz, M. Klata et al, Determinants and disparities in access to pediatricians in Poland, April 2022
- ^
workforce consensus: UK overview report. RCPCH, 2019
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
Y Zhang, L Huang, X Zhou et al. Characteristics and workload of pediatricians in China. 2019
- ^
BB Shehu, EA Ameh, poverty and disease burden vs medical education in sub-saharan Africa, 2007
- ^
F. Mullan, S. Frehywot, F.Omaswa et al.medical schools in sub-saharan Africa, 2011
- ^
- ^
Y Zhang, L Huang, X Zhou et al. Characteristics and workload of pediatricians in China. 2019
- ^
Z.Yuan, L.Chuzhi, X. Wenfeng et al. The study on the relationship between job burnout and social support of pediatrician in Guangzhou, 2022
- ^
Z.Yuan, L.Chuzhi, X. Wenfeng et al. The study on the relationship between job burnout and social support of pediatrician in Guangzhou, 2022
- ^
Xf. Xu, Xy. Sun, Lz. Du. A comparative analysis of clinical operation system and continuing education of pediatricians between Chinese and American Children’s Hospital, 2019
- ^
Af.He, An analysis on sources of stress and management on of clinical pediatrician, 2021
- ^
- ^
- ^
Dyson foundation CPTI
- ^
H. Zar, A. Vanker, D. Gray et al. The African Pediatrics Fellowship Training Program in Pediatric Pulmonology: A model for growing African Capacity in Child Lung Health, 2017
- ^
- ^
H. Zar, A. Vanker, D. Gray et al. The African Pediatrics Fellowship Training Program in Pediatric Pulmonology: A model for growing African Capacity in Child Lung Health, 2017
- ^
- ^
H. Zar, A. Vanker, D. Gray et al. The African Pediatrics Fellowship Training Program in Pediatric Pulmonology: A model for growing African Capacity in Child Lung Health, 2017
- ^
theapfp.org
- ^
Dr S. Clark, Dr R. Cheung, State of Child health 2020 - England, RCPCH
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
C Chen, P Qihua et al. Developing community pediatrics in China: necessity, feasibility, and recommendations derived from the US training system for community pediatricians, 2021
- ^
B.Harper, W. Nganga, R. Armstrong, et al. Where are the pediatricians? An international survey to understand the global paediatric workforce, 2018
- ^
C Chen, P Qihua et al. Developing community pediatrics in China: necessity, feasibility, and recommendations derived from the US training system for community pediatricians, 2021
- ^
Dr S. Clark, Dr R. Cheung, State of Child health 2020 - England, RCPCH
- ^
Y Zhang, L Huang, X Zhou et al. Characteristics and workload of pediatricians in China. 2019
- ^
Y Zhang, L Huang, X Zhou et al. Characteristics and workload of pediatricians in China. 2019
- ^
Unicef, Children in Africa, key statistics on child survival and population
