This research project was commissioned by Flourishing Minds Fund and created by CEARCH. It consisted of a review of the available literature on mental health and consultation with over a dozen experts in the field. The full report can be found here.
Key Findings
- Mental illness forms 3% to 16% of the global disease burden, depending on how mental health is categorized
- The data on mental health prevalence is unreliable, especially in LMICs. But mental illness appears to be a major problem everywhere in the world. We suspect that geographical variation in mental illness is usually not one of the top considerations when deciding where to implement an intervention.
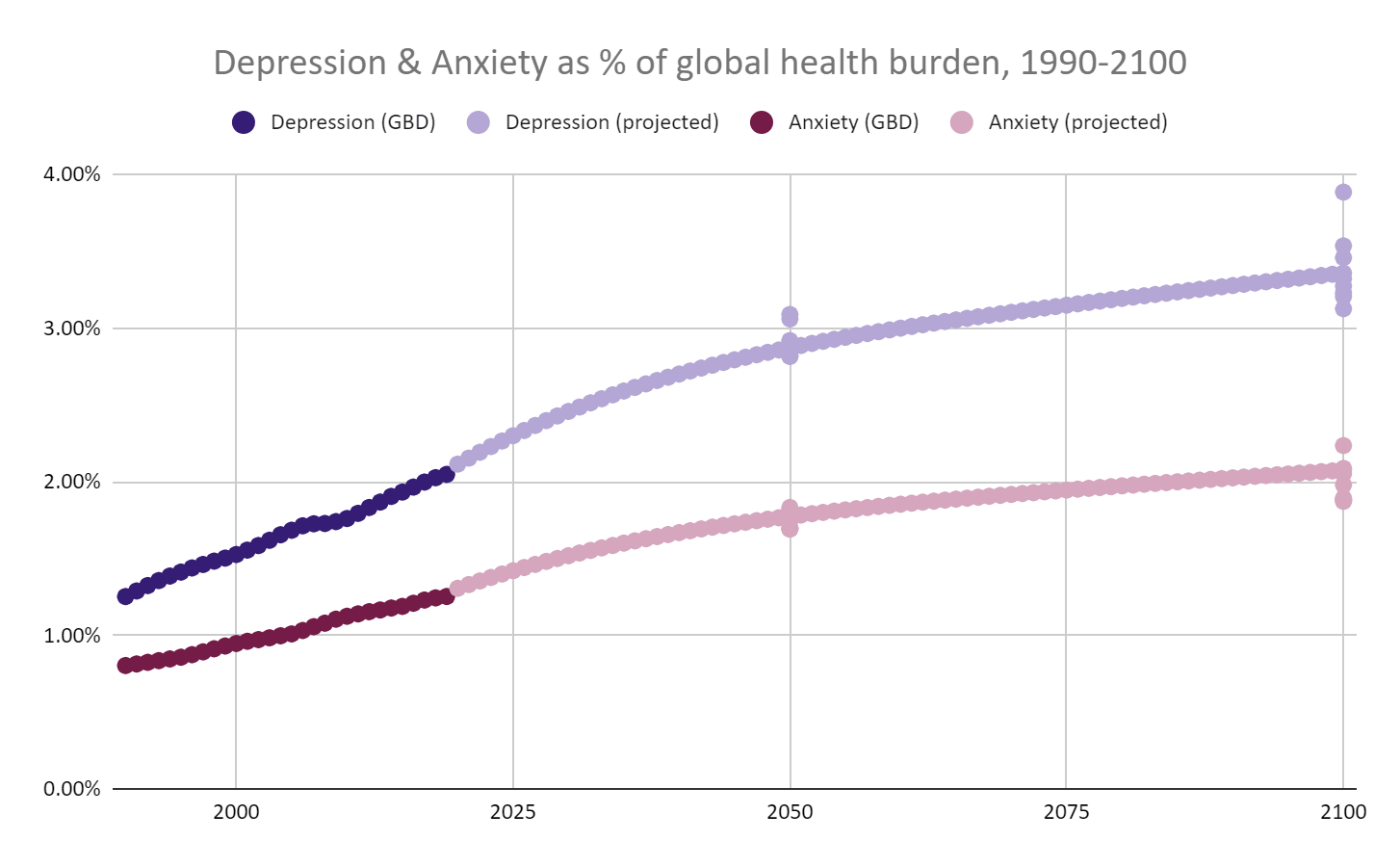
- As we continue to make progress against communicable diseases and poverty, mental illness will become a larger proportion of the total disease burden over time. We estimate that the relative importance of depression and anxiety will increase by 50% by the end of the century
- The nature of the burden will change over time. Conditions affecting the elderly will become a bigger problem, and we may see an increase in mental illness among adolescents.
- We don’t know much about how to address mental illness in resource-poor societies. Further research is likely to pay dividends in the coming decades.
What counts as mental illness?
Mental illness can be categorized in a number of ways. In general this report focuses on mental health conditions that are less likely to fall under the remit of typical “Global Health and Development” work. Hence we exclude conditions that are tightly linked with infectious disease, exposure to toxic chemicals, and malnutrition (such as IDID, which IHME class as a mental disorder). We also choose to exclude neurodevelopmental and childhood-behavioral disorders such as Autism and Conduct Disorder on the basis that they are slippery conditions which are very poorly understood. We focus more heavily on conditions with a lower degree of heritability.
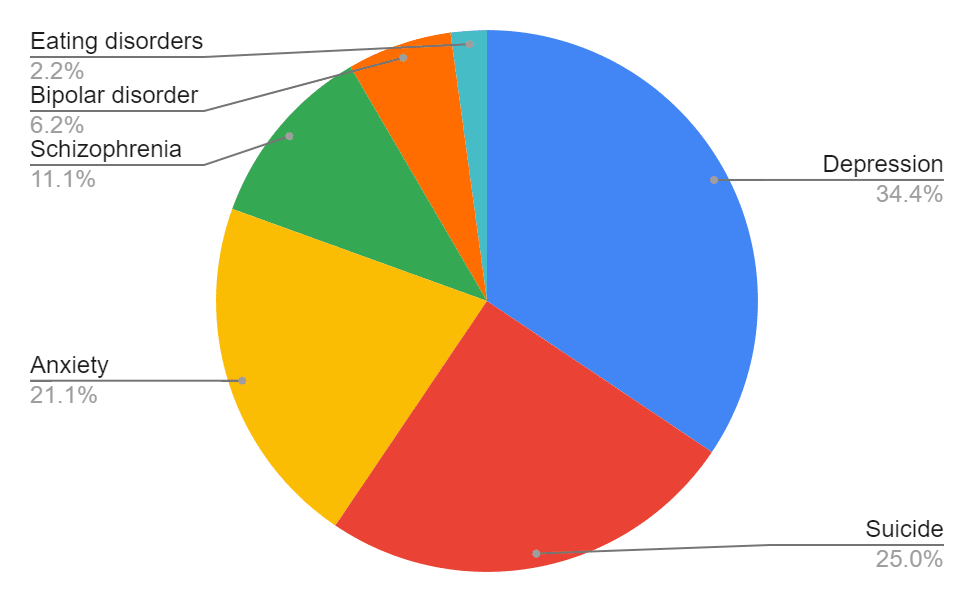
We include suicide on the assumption that suicide and self-harm are primarily caused by mental illness, unhappiness and despair. Suicide is not classed as a mental disorder in the GBD study. I have used the GBD figures for “self-harm”, the burden of which is almost all attributable to premature death.
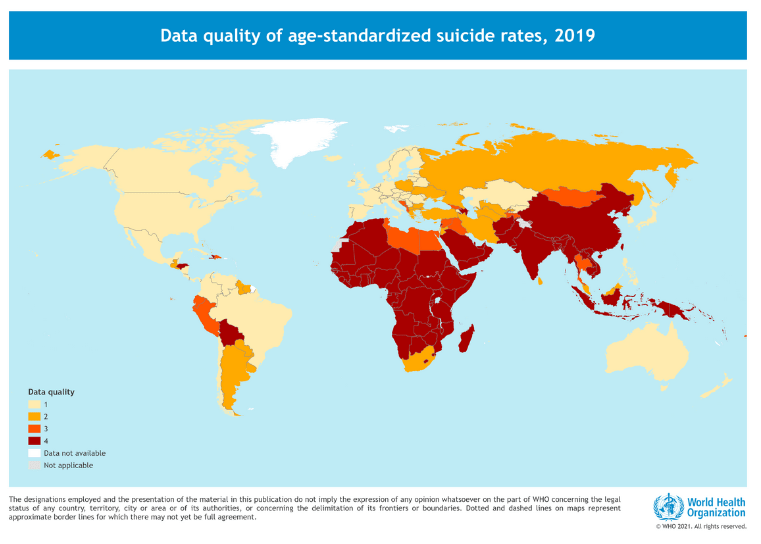
Most of this sequence focuses on the conditions in the table below (all figures extracted from GBD, 2019).
Above: the burdens of six mental health phenomena. Heritability is a measure of how strongly the prevalence of the condition is explained by genetic factors[1].
Scale of the Problem
Summary:
- The burden of mental illness is huge
- The economic effects are also huge, but poorly understood
- Healthcare spending does not match the size of the problem
Mental illnesses impose an enormous health and economic burden worldwide. The conditions in the table above account for 5.4% of the total DALY burden of all causes of death or injury in IHME’s Global Burden of Disease (GBD) study, which is comparable to the combined burden of HIV/AIDs, Malaria and Tuberculosis. A study by Arias et al. (2022) cast the net wider by including substance abuse, neurological and neurodevelopmental disorders, and by considering the increase in premature mortality and chronic pain. Together this accounted for 16% of the total DALY burden.
The economic impact is also enormous. Mental illness can impact education, employment, absenteeism and productivity. It imposes healthcare costs, too. Since mental illness is more likely than most conditions to affect people of working age, and much mental illness goes untreated, we suspect that the economic costs of stem more from lost productivity than healthcare.
Beck et al. (2011) identify a strong link between depressive symptoms and productivity, and a 2011 report by the World Economic Forum identifies mental illness as the biggest source of lost productivity due to disability. The report estimates that global economic loss due to mental illness was $2.5 trillion in 2010 (3.8% of global GDP), and projects that by 2030 the economic toll of mental illness will be “greater than that of cancer, diabetes, and respiratory ailments combined”.
However, healthcare spending does not correspond to the size of the problem. “High-income countries allocate about 5.4% of their total government health expenditure to mental health, compared to 1.7% in LMICs — and only 0.02% in the nine low-income countries covered by the WHO mental health Atlas” (WHO, 2021, quote from Banerjee et al., 2022). India allocated just 0.8% of its 2022 healthcare budget to mental health, representing about USD 0.06 per citizen. This means that mental healthcare costs are often borne out-of-pocket or by private insurance, and that those who cannot afford it are simply left untreated.
Mental health conditions may be seen (with some justification) as more intractable than key physical conditions, especially in poor countries where preventable infectious diseases are common. This may partly explain the gap between funding and burden. It also underlines the urgent need to find cost-effective ways of tackling mental illness so that philanthropic, private and public funding can be better put to use.
The burden is uncertain, and may be underrated
The global burden may be underrated for a number of reasons.
- Mental illness is often less visible than physical illness, which makes underdiagnosis and misdiagnosis more likely
- Medical mental health provision, and the quality of diagnosis and record-keeping, varies widely between countries. Statistical methods are used to estimate the burden in regions with scarce data, which could lead to large errors (see the next post in this sequence for more on this)
- The QALY and DALY weightings of health conditions are derived from the judgments of ordinary people, who may systematically underrate mental illnesses. Bounded measures such as QALYs and DALYs may fail to capture states of extreme suffering associated with severe mental illness (see the next post in this sequence)
Geographical Distribution
Summary:
- The burden of mental illnesses appears to be high everywhere, with relatively modest differences between countries
- Overall we suspect that geographical distribution should not be the main concern when determining where to do an intervention. The ease and cost of operating are probably much more important concerns.
- Data from the GBD study and the WHO should be seen as unreliable, especially data on LMICs
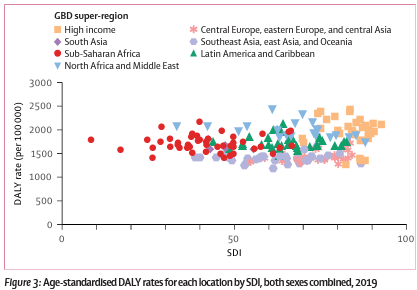
Results from the Global Burden of Disease (GBD) study suggest that the total burden of mental disorders does not vary widely between countries. The vast majority of countries have an age-standardized burden of between 1250 and 2500 DALYs per 100,000.
The chart above displays the burden from mental disorders in the GDB study, with each country represented by a dot. Note that this report uses a different categorization of mental illness.
The chart above suggests that the burden is lower than average is South Asia, and higher than average in most HICs. However, the extrapolation methods used in the GBD - demographically similar countries are assumed to have similar disease profiles - probably exaggerates similarities within categories. In fact, we think the unreliability of the results is sufficient to potentially negate or even reverse the trends we see in the data (see Data quality).
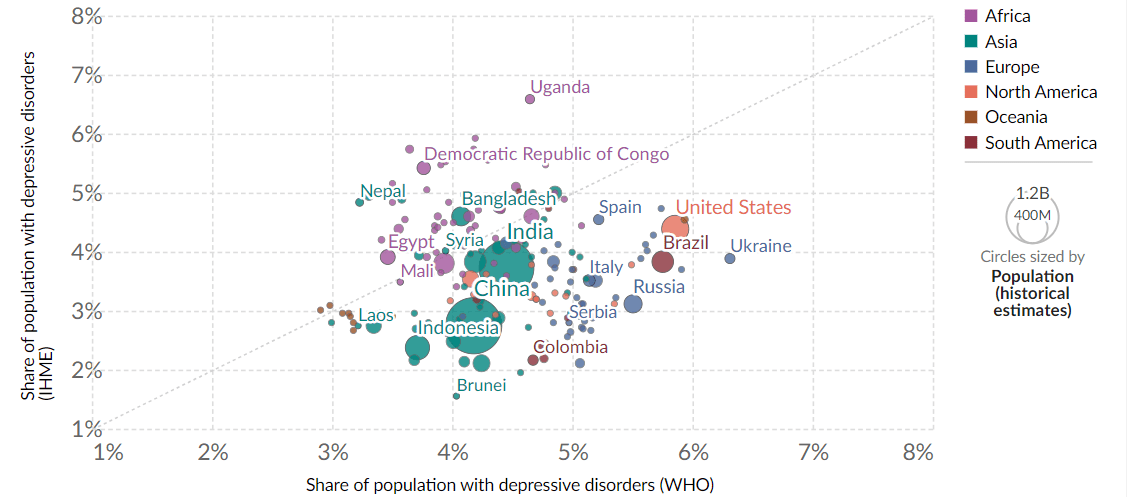
As an indication of the unreliability of the data, we can compare the GBD data against that of the WHO’s Global Health Observatory (see chart below). The two sources disagree on the prevalence of depressive disorders (probably the most-studied mental disorder), with several estimates diverging by more than a factor of two. The GBD estimates higher depression rates than the WHO does in Africa, and lower rates in Asia and HICs (OWID, 2022).
Taking the GBD results at face value, we find that anxiety has moderate positive correlation with log(GDP per capita) (OWID, 2019a), while depression has moderate negative correlation with log(GDP per capita) (OWID, 2019b). In other words, weather countries have more anxiety and less depression than poor countries. However, the scale of the effect of wealth is modest in both cases: the expected difference in anxiety/depression between the wealthiest and poorest countries is no more than 2×.
Several experts told us that finding people in need of mental health treatment is not a major challenge in LMICs. With a good screening process, it should be possible to target sufferers of depression and other mental illnesses in any region. Other considerations such as cost, quality of existing healthcare, infrastructure and availability of labor are likely to be far more important than local disease prevalence.
There are some exceptions to this rule:
- Population-level interventions such as policy advocacy. These primarily have fixed costs, and are more promising when the number of potential beneficiaries is high
- Instances when the mental disorder is likely to be highly localized, such as PTSD in the aftermath of a civil war.
Change over time
Summary
- There are signs that the per-capita mental health burden is increasing
- As we make progress in other areas of global health, mental illness’ share of the total burden will grow
- We estimate that the relative importance of depression and anxiety will grow 50% by the end of the century
- Mental illnesses associated with the elderly will increase in importance as populations age
- It is possible that adolescent mental health will deteriorate as countries develop
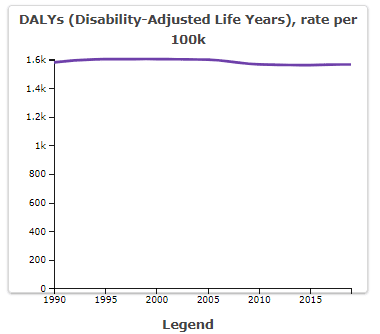
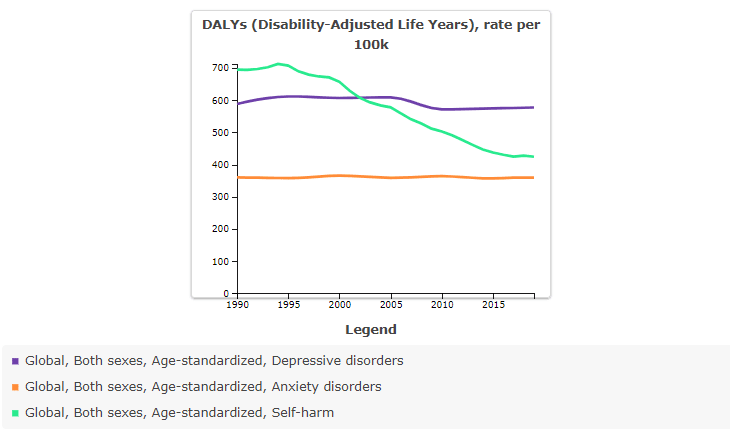
The GBD study suggests that the burden of mental illness remained stable between 1990 and 2019. The graph below shows the age-adjusted global burden of mental disorders.
This result should be taken with a heavy pinch of salt. We can see from the chart below that the prevalence of suicide[2] (not classified as a mental disorder in the GBD) varied far more than anxiety or depression, which are harder to diagnose. We strongly suspect the apparent stability of the mental health burden reflects modeling choices rather than underlying trends.
We suspect that the GBD is doing a poor job of detecting changes in the mental health burden over time. However we are more confident in their assessments of other health conditions, and this data suggests that mental health will increase in relative importance over time.
Depression and Anxiety will probably become more important
Summary
- The poor quality of available data makes future projection very uncertain
- As we make progress against poverty and communicable diseases, mental health will increase in importance
- Depression and anxiety alone may account for 5% of the global disease burden by the end of the century
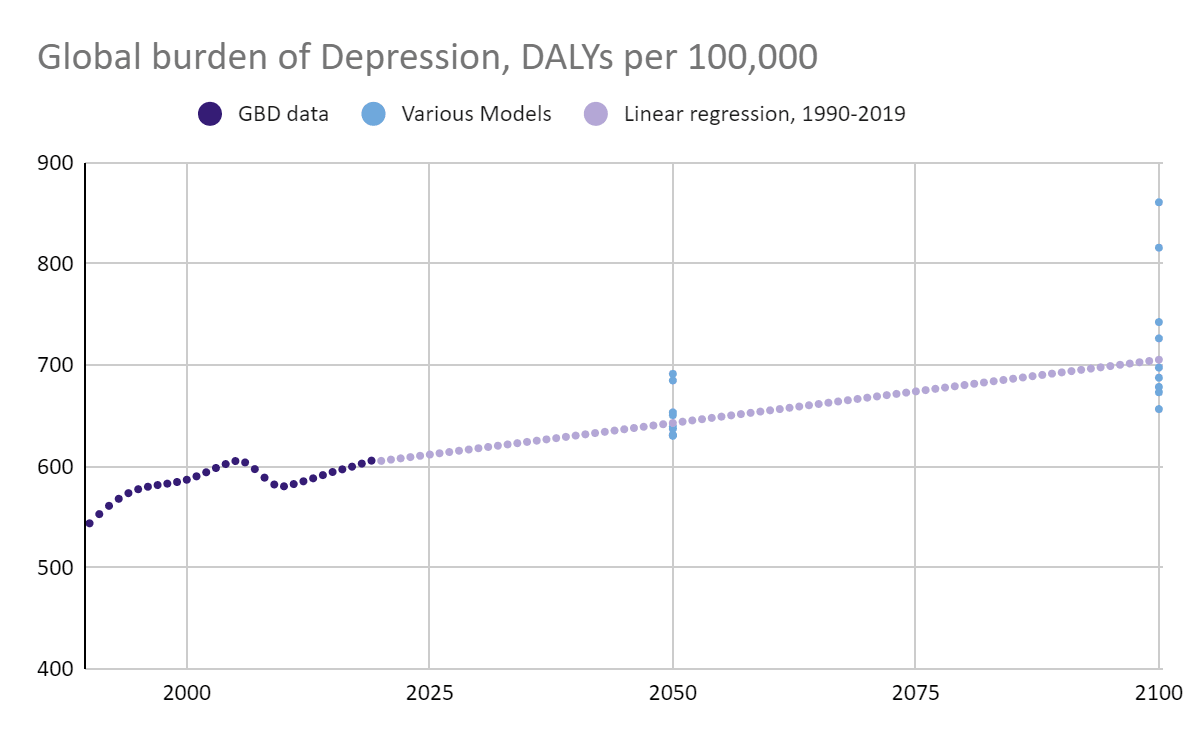
According to the GBD survey, the period 1990-2019 saw depression rise, then fall, then rise again. Given the sparsity of data from many countries, we are very skeptical that this data represents real fluctuation (see Data quality below). It is more likely the result of tweaks and improvements in the way GBD handles data, and of the increase in data coming in.
Nevertheless, we can attempt to extrapolate into the future. A linear regression model suggests that the burden of depression will increase from 600 to 700 DALYs per 100,000 by the end of the century. The blue dots in the graph below are products from various linear and exponential models based on the 1990-2019 data.
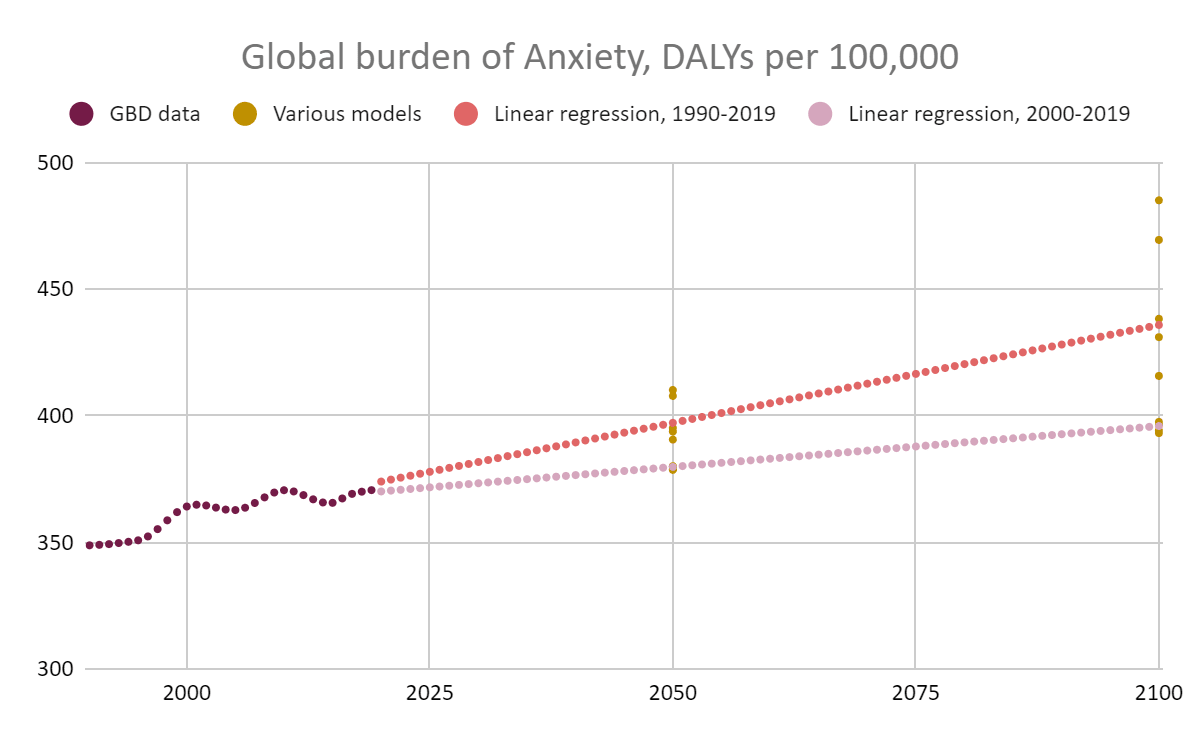
Applying a similar method to the anxiety data, we predict that the burden will increase from 370 to over 400 DALYs per 100,000 by 2100. The pink data points represent a linear regression based on the 2000-2019 data only.
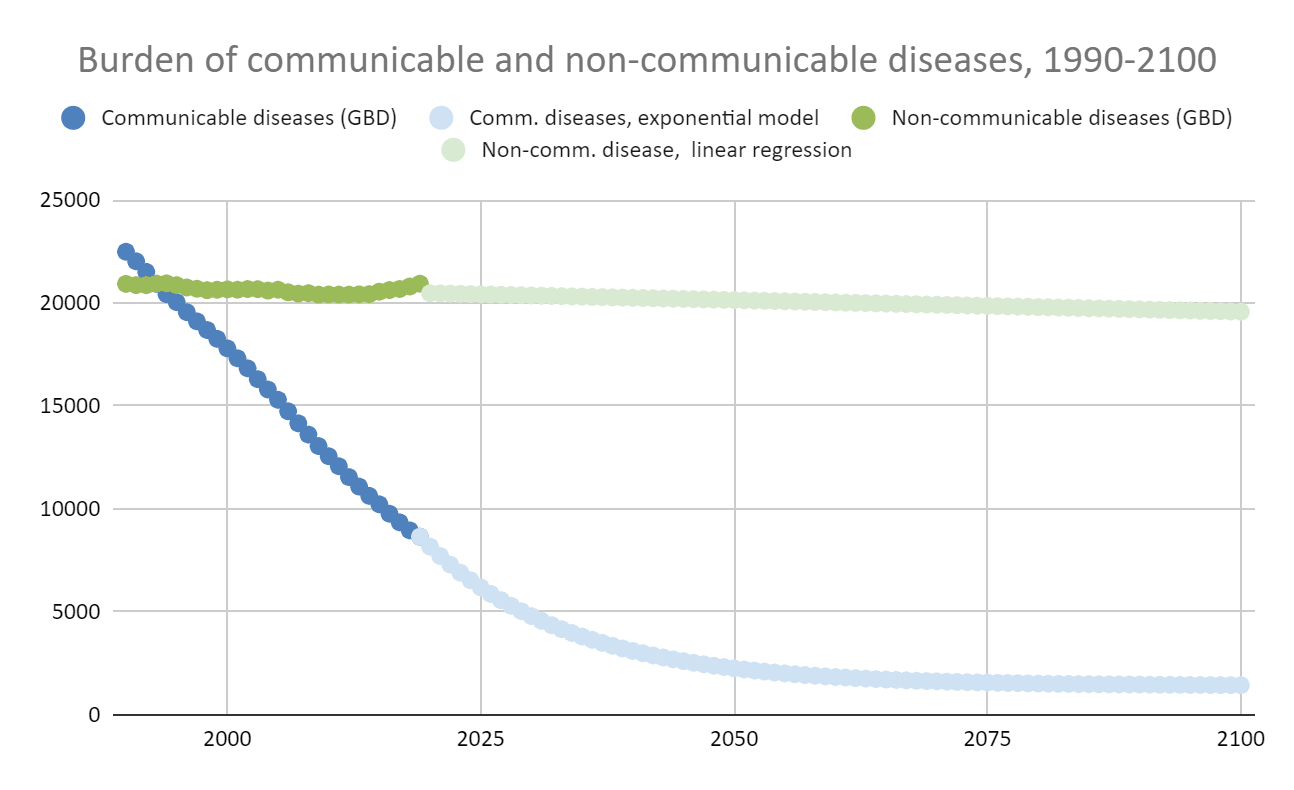
While the projected increases in the burdens are modest, they should be understood in the context of the decreasing global disease burden. The burden from communicable, maternal, neonatal, and nutritional diseases plummeted in the period 1990-2019, while the burden from non-communicable diseases remained stable.
By projecting the burden of communicable and non-communicable diseases into the future[3], we can estimate what proportion of the disease burden will be attributable to depression and anxiety.
We find that depression is projected to go from 2% to over 3% of the total disease burden by 2100, while anxiety will go from 1.3% to approximately 2%. Thus we expect the relative importance of depression and anxiety to increase by about 50%.
The raw data from the graphs in this section can be found here.
This phenomenon - an increase in the relative importance of mental illness as we make progress against communicable diseases - may be even more pronounced in poor countries, where the communicable disease burden is high and (usually) falling fast. A case can be made for funding research that increases our ability to tackle mental illness in the future, even if the interventions in question are not yet cost-effective. As explored in the final post in this sequence, we don’t know how best to tackle mental illness in poor countries. Increasing the evidence base will allow us to work more effectively when mental illness moves up the agenda.
One notable exception may be suicide. The suicide rate dropped by 29% between 1990 and 2019. Rapidly industrializing countries that once had above-average suicide rates have seen significant drops, as in China (53% drop) and India (22% drop). This is probably partly due to stricter controls on the most toxic pesticides. Although many countries still have insufficient restrictions, most of the available gains may already have been realized (see the final post in this sequence).
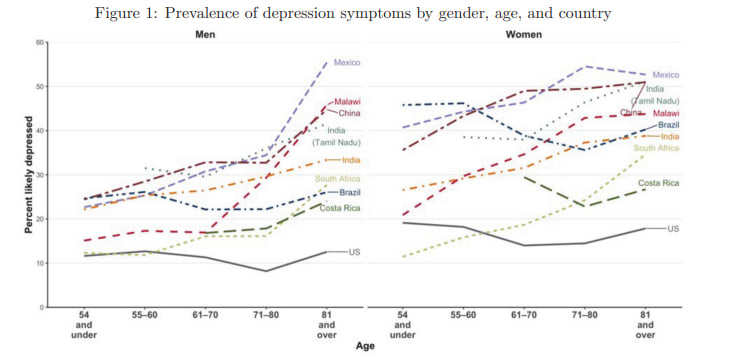
Conditions affecting the elderly will become more important
We can expect the nature of the mental illness burden to evolve as the population ages. Against popular perception, there are signs that loneliness and depression among the elderly is more prevalent in LMICs than in HICs. Banerjee et al, (2022) compared results from a group of surveys in seven LMICs and the US. They found that over-55s in the LMICs were much more likely to be depressed than their US counterparts, although the survey types and diagnosis thresholds differed between countries, making comparison fraught[4]. The study drew from the 2016 wave of the US Health and Retirement Study (HRS) and conducted “HRS-style” surveys in the LMICs. Cut-off points differed by country based on what has been found to maximize sensitivity and specificity in different contexts. We suspect this partly explains why prevalence of depression seems to be far higher (3.2% across the global adult population, according to the GBD).. What we can say with more certainty is that depression appears to become more prevalent above the age of 70 in LMICs, but not in the US.
In all countries, functional impairment, loneliness and living alone were strongly correlated with depression. Higher prevalence of these indicators seems to account for some of the depression gap between the US and the LMICs, but probably not all of it. It seems plausible that poverty, untreated pain and lack of access to transport and communication could also be causal factors.
Old social norms of caring for elderly neighbors and relatives are breaking down at a time when the elderly population is steadily growing. It seems plausible that government policy should step in to plug the gap. Long-term mental health policy would benefit from a better understanding of the determinants of mental illness among the elderly and the interventions that can mitigate it. Banjeree et al, say their evidence “suggests that policies to lower poverty and financial strain might go a long way toward reducing depression and improving psychological well-being more broadly (for example, via pensions)”. Technology may give the elderly relief from loneliness, and we may benefit from new interventions aimed at an increasingly tech-literate elderly population.
Adolescent mental health may deteriorate
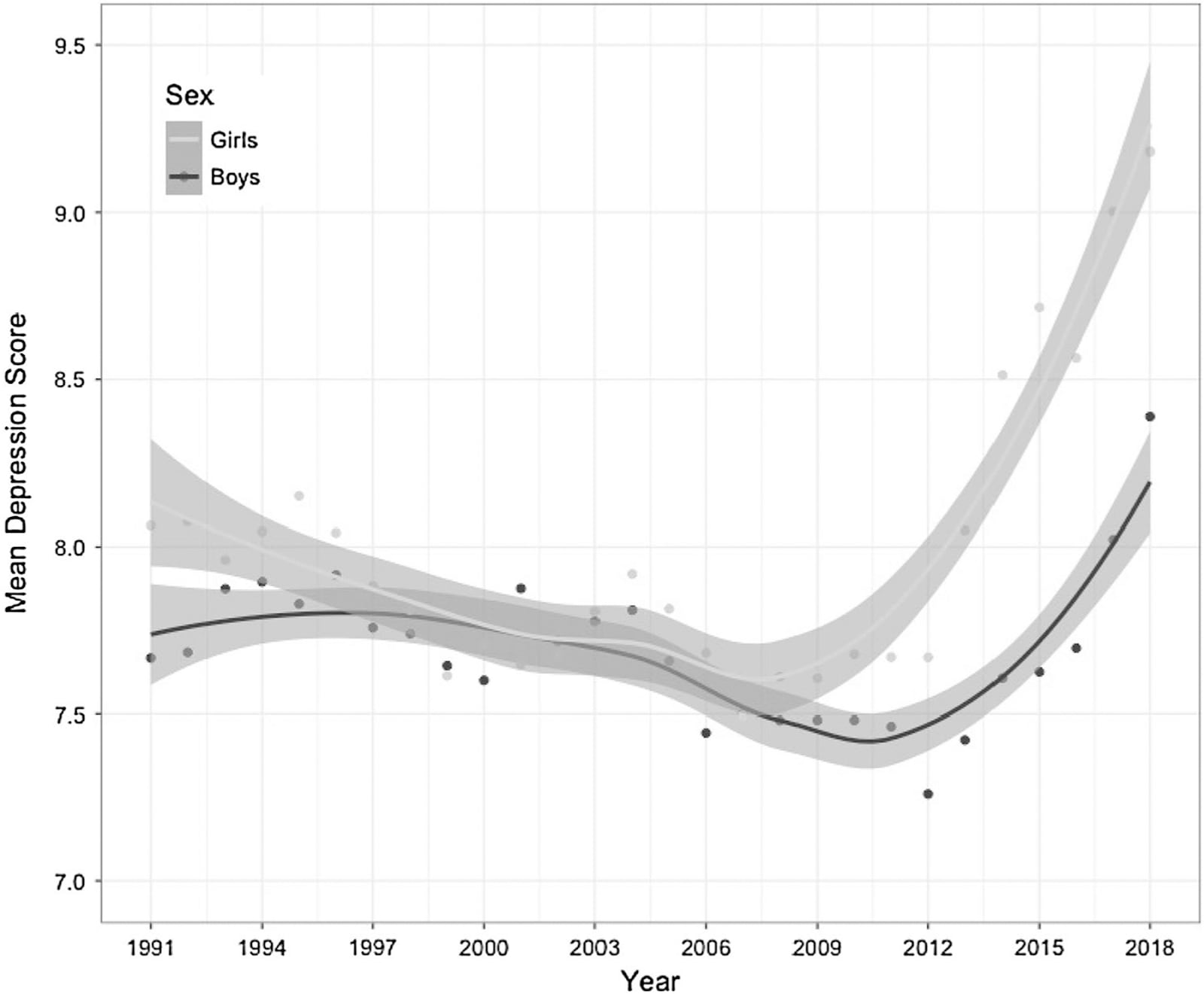
If the population is aging, can expect interventions aimed at children and mothers to decline in relative importance? It’s possible that early-life mental health interventions are underrated (see the final post in this sequence for more on this). It’s also possible that youth mental health is worsening over time. This is a very slippery concept: many people believe that there is a youth mental health crisis of depression, anxiety and eating disorders, perhaps fueled by social media. However, any observed increase could be the result of the increasing awareness of mental health over time.
Birth cohort studies attempt to cut through changes in culture and awareness by surveying successive generations using the same methods. The results from two US studies imply a significant deterioration in youth mental health in the second half of the 20th century. Twenge (2000) saw anxiety and neuroticism among children and college students increase by about one standard deviation between 1953 and 1993. In a more expansive study spanning 1938 to 2007, Twenge et al. (2010) found that “[t]he current generation of young people scores about a standard deviation higher (average d = 1.05) on the clinical scales, including Psychopathic Deviation, Paranoia, Hypomania, and Depression.”
A more recent cohort study by Keyes et al (2019) observed an uptick in depressive scores among US adolescents in the 2010, especially among girls.
Mean depressive affect symptoms by year among US adolescent girls and boys, 1991–2018. The standard deviation of scores is approximately 4.
We simply don’t have birth cohort data of this quality from LMICs. If the factors contributing to youth mental illness are tied in with development, we can expect youth mental health to deteriorate in the coming century.
Data quality
GBD study data
There are a number of reasons why estimates of the mental health burden in LMICs could be highly inaccurate, especially in LMICs:
- Mental illnesses are difficult to diagnose consistently between countries
- Mental health data is scarce in LMICs
- Studies in LMICs are often smaller and have less representative samples
- Diagnosis tools are usually developed in the West, and thus cultural differences may make them less powerful in other regions
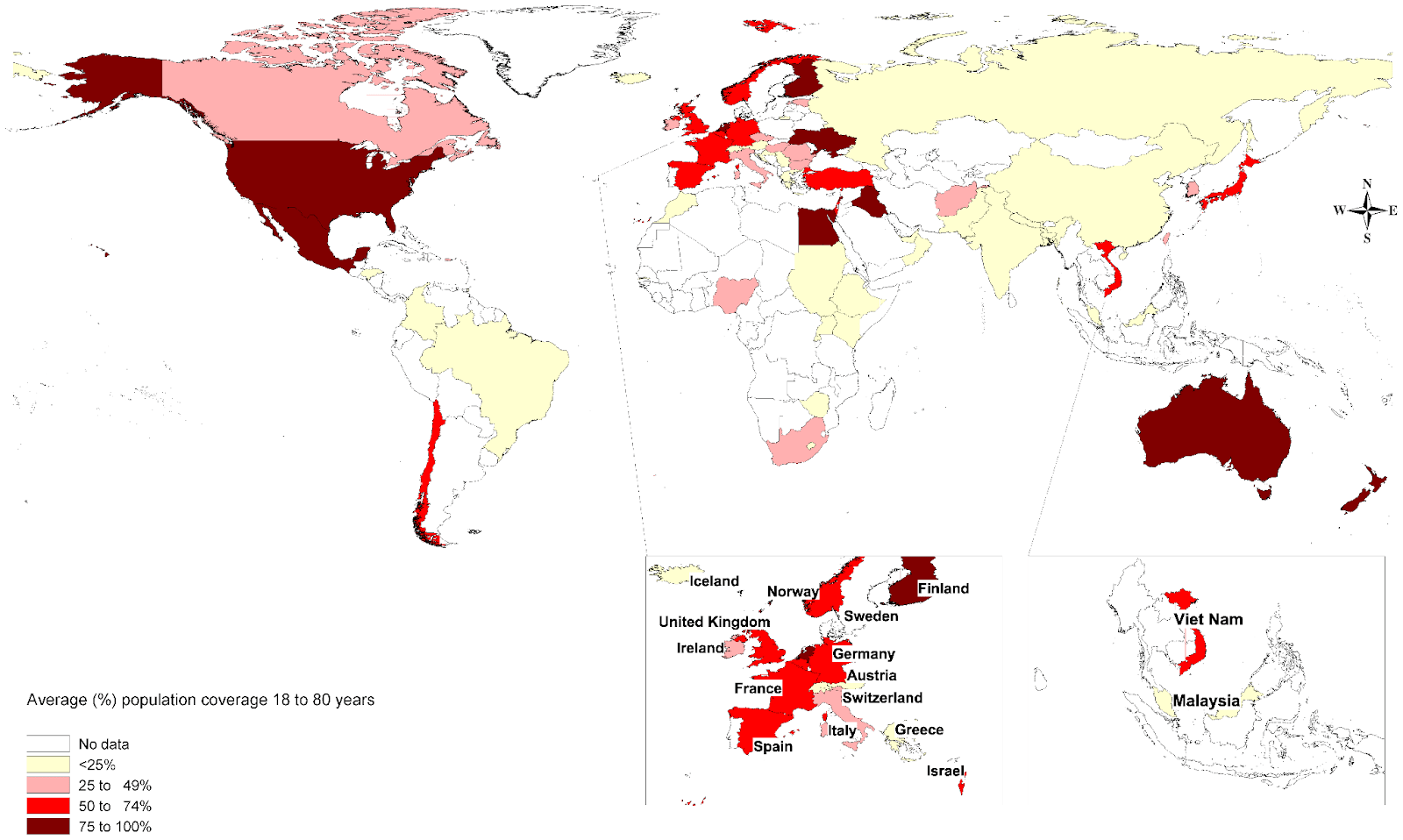
The GBD attempts to piece together evidence to estimate disease burdens in every country, but the lack of comprehensive data means that IHME uses statistical techniques to fill the gap. For example, depression is the mental disorder with the broadest evidence base, but the GBD only has primary sources from 111 countries (IHME, 2019). This means that dozens of countries are not represented at all.
From the map below we can see that depression and anxiety data from most LMICs is sparse or non-existent. Coverage of East, Southern and Central Sub-Saharan Africa, and South Asia is pitifully low[5] (IHME, 2008).
Population coverage of prevalence data for common mental disorders: averaged across major depressive disorder, dysthymia and anxiety disorders (Baxter et al., 2013).
In regions where the data is sparse or non-existent, IHME extrapolates based on other data such as age sex and risk factors.
Adding to the difficulty is the fact that the available sources are often not easily comparable. From some countries the data may come from clinical diagnoses and health insurance claims, in others they may come from layperson-administered surveys (OWID, 2023). In general, LMIC data is less likely to involve clinical diagnosis, and is more likely to involve smaller, less representative samples. Between countries, different definitions of mental health conditions and different clinical practices make cross-comparison even more difficult.
IHME attempts to account for all of these factors with statistical adjustments. This is a huge challenge, and it seems probable that IHME’s stated confidence intervals are too optimistic.
For example, the IHME estimates the age-adjusted prevalence of Schizophrenia at 241 and 434 per 100,000 in Denmark and the USA respectively. This seems implausible, given that the condition is believed to be ~79% heritable (Hilker et al., 2018).
It is possible that the prevalence of depression and anxiety in LMICs is radically different from what is found in the GBD results. Experts have suggested that diagnosis methods and surveys developed in the West may have limited utility in other cultures, where MH conditions manifest differently. For example, a doctor in Sub-Saharan Africa suggested to us that patients who seek medical help for physical aches and pains are often found to be suffering from depression. People largely engaged in domestic or manual labor may be less likely to notice “struggling to concentrate” (often used as a key symptom of depression) than white-collar workers in HICs. Hence cultural differences may be leading to under-diagnosis in non-Western societies.
Depression data
In general, the data on depression prevalence is based on clinical diagnoses in HICs, and questionnaire data in LMICs. Questionnaires are usually more sensitive, so the prevalence rates that spring from the two methods are not directly comparable. The IHME attempts to use statistical adjustments to account for the differing sensitivity levels, but it is unclear how reliable the results are.
Layperson-administered survey methods have been applied in both HIC and LMIC settings, which can in theory enable us to compare depression rates more directly. However, these studies usually examine small, unrepresentative samples. A meta–analysis by Bello et al. (2022) of depression studies conducted in Africa during the Covid pandemic detected depression prevalence ranging from 8% to 80%. Two studies conducted in the same country found prevalence levels of 13% and 83% respectively. Data from the United States National Health and Nutrition Examination Survey (NHANES) is probably far more representative than the studies from Africa. Tomitaka et al. (2018) find that PHQ-9 scores from the NHANES “exhibited an exponential pattern, except at the lower end of the distribution” (Tomitaka et al., 2018). Most scores were under 5 (out of 27), and there was a long right tail of higher scores. Unfortunately, without large, representative studies in poor countries, we are unable to “directly” compare PHQ-9 scores between rich and poor countries.
Even if we had better studies, it is possible that our diagnostic tools are less reliable in non-Western societies. One expert suggested to us that depression manifests differently in different cultures, and hence Western-developed diagnosis tools can under-diagnose when applied in other settings. Scorza et al. (2018) examined data from the World Mental Health Surveys, a series of studies aimed at predicting prevalence of mental disorders across 27 countries. They found that the estimated depression prevalence in the Nigeria sample was sever times higher when using a Latent Transition model instead of the algorithm used by the WMHS. Prevalence estimates in the US and New Zealand barely changed under the different model. This illustrates just how sensitive measurement methods our estimates are.
Suicide data
We are doubtful that the IHME will be able to model suicide in LMICs accurately, given the complex factors that affect suicide rates and the reliability of available data. Suicide appears to have a strong cultural component which may not be captured by the demographic factors used in extrapolation. For example, suicide rates appear to be lower in religious societies, but it is unclear how much of this is attributable to underreporting vs. actual lower prevalence. Many LMICs have criminalized suicide, which makes accurate measurement near-impossible. Experts told us that many suicides are not reported, and that police and medical authorities often keep separate suicide records without cross-referencing.
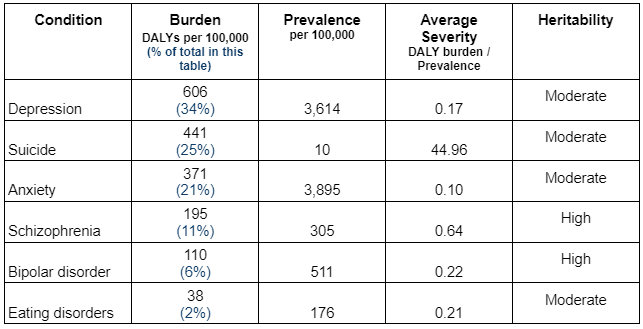
The WHO provide a map (below) which illustrates the suicide data gap in LMICs (A score of 1 denotes high-quality data).
Anyone considering a suicide intervention in an LMIC should not complacently rely on official data. The Centre for Pesticide Suicide Prevention know this: they combine data from police reports, health services and local surveys in order to build their own best guess.
Is the LMIC burden underrated?
For anyone who wants to combat mental illness, the precise scale of the mental health burden in LMICs is not particularly important. We are confident that people suffer from mental illness all over the world, and that people in poor countries are both less likely to have access to treatment, and are cheaper to treat. Hence as a general rule interventions targeting mental illness in LMICs will be more cost-effective than those in HICs.
However, scale is important if we wish to determine how much of the limited resources available in LMICs should be allocated to mental health. Unfortunately, we feel that there is not enough data to determine with confidence whether the mental health burden in LMICs is underrated.
Reasons why the burden of mental health may be underestimated in LMICS:
- Diagnostic criteria and tools are largely developed in the West. When applied in culturally different contexts, they may be less sensitive to mental illness
- Awareness of the importance of mental health is considered to be worse in LMICs. This may cause people to ignore mental health problems, or to ascribe symptoms to physical or spiritual causes.
- Our health metrics (such as the QALY and DALY) may generally underrate the badness of mental illness compared to other conditions, as explored in the next post in this sequence.
Reasons why the burden of mental health may be overestimated in LMICS:
- Researchers may be motivated to exaggerate the prevalence of mental illness in LMICs in order to raise the profile of this neglected field
- Many symptoms that in wealthy countries are signs of mental illness may in LMICs be the product of poverty. Poor sleep and trouble concentrating, for example, are symptoms of depression but could also be caused by malnutrition.
Critical research gaps
We need research to improve our understanding of the burden of mental illness, especially in LMICs.
- Studies that use identical (and more culturally-neutral) methods and representative samples to estimate the prevalence of mental illnesses in both wealthy and poor countries
- Investigations into the different manifestations of depression and other mental illnesses in specific LMIC settings
Conclusion
Mental illness imposes an enormous burden. It inflicts misery and reduces productivity around the world. However, a lack of reliable data makes it difficult to pinpoint precisely how bad the toll is, and makes it almost impossible to trace how it is changing over time. Improving the quality of this data will be instrumental at improving our powers of tackling mental illness.
We can be confident that depression, suicide and anxiety are the greatest sources of mental health burden. These conditions are correlated with each other and contribute to each other, and work on one condition is likely to mitigate the others.
As we make progress against communicable diseases, and as the average age rises, mental health is projected to become a larger share of the disease burden. As the easiest-to-prevent physical illnesses fade away, mental illness interventions will become more cost-competitive.
We can expect the nature of the burden to evolve, and the problems of loneliness and depression among the elderly to become more important. But there are also indications that youth mental health has been deteriorating in wealthy countries. If this trend holds true in developing countries, we can expect disorders of adolescence to become a larger problem.
- ^
Broadly, less-heritable illnesses are better targets for preventative interventions, and may be more easily “cured” by treatment interventions. This is largely why this report does not explore interventions aimed at Schizophrenia and Bipolar disorder.
- ^
The GBD measures “self-harm”, not suicide. Since the vast majority of the self-harm burden comes from deaths, we treat the GBD’s self-harm figures as equivalent to suicide in this report.
- ^
We use a linear regression model with the non-communicable disease data. This is not possible with the communicable disease data, as it would soon lead to impossible negative values. Instead, we assume a “constant + exponential” model, where the constant part is 1400 DALYs per 100,000, which is the rate in modern-day high SDI countries, according to the GBD survey.
- ^
The study drew from the 2016 wave of the US Health and Retirement Study (HRS) and conducted “HRS-style” surveys in the LMICs. Cutoff points differed by country based on what has been found to maximize sensitivity and specificity in different contexts. We suspect this partly explains why prevalence of depression seems to be far higher (3.2% across the global adult population, according to the GBD).
- ^
The data in the map is dated and the GBD appears to draw from more sources now. However, the data gap between rich and poor countries remains.