This research project was commissioned by Flourishing Minds Fund and created by CEARCH. It consisted of a review of the available literature on mental health and consultation with over a dozen experts in the field. The full report can be found here.
Key Findings
- Cost is a very important variable in assessing mental health interventions, and it can vary widely
- Interpersonal group therapy is a promising way of improving mental health provision in poor countries, although the scale of the effect of psychotherapy is unclear. Technology may allow psychotherapy to be delivered more cheaply and at scale.
- Tackling risk factors can prevent mental illness. Policy advocacy could be a good lever for doing this.
- Suicide prevention appears to be highly neglected in poor countries.
- Mental illness will increase in relative importance over time, so we should place a premium on any work that increases our understanding of how to mitigate it
Report Structure
- Executive Summary
- Mental illness is growing as a proportion of the global disease burden
- Does a DALY approach underrate the badness of mental illness?
- An overview of promising mental health interventions
- Treatment interventions
- Prevention interventions
- Intervention BOTECs
Executive Summary
Burden
Data on the burden of mental health is unreliable, especially in low-middle income countries (LMICs). The IHME’s Global Burden of Disease (GBD) study simply has no data from many poor countries. When they do have data from a low-income country, it is more likely to come from small, unrepresentative samples and less likely to come from expert diagnosis.
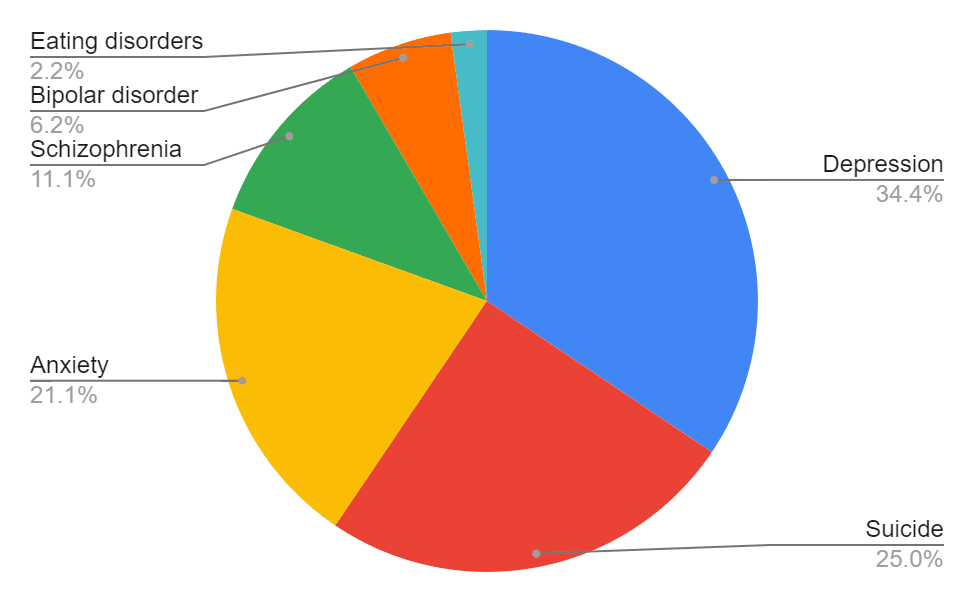
However, we can be confident that mental illness is a big problem. Depending on how “mental illness” is defined, it represents between 3% and 16% of the total disease burden. This report focuses on the conditions in the table below, which account for 5.4% of the global disease burden.
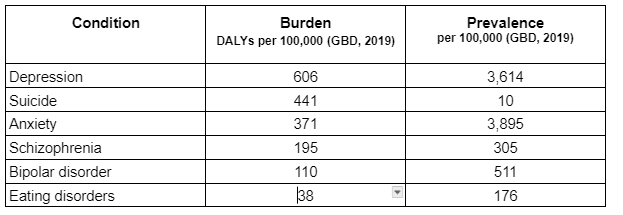
Relative burden attributable to six key conditions (GBD, 2019)
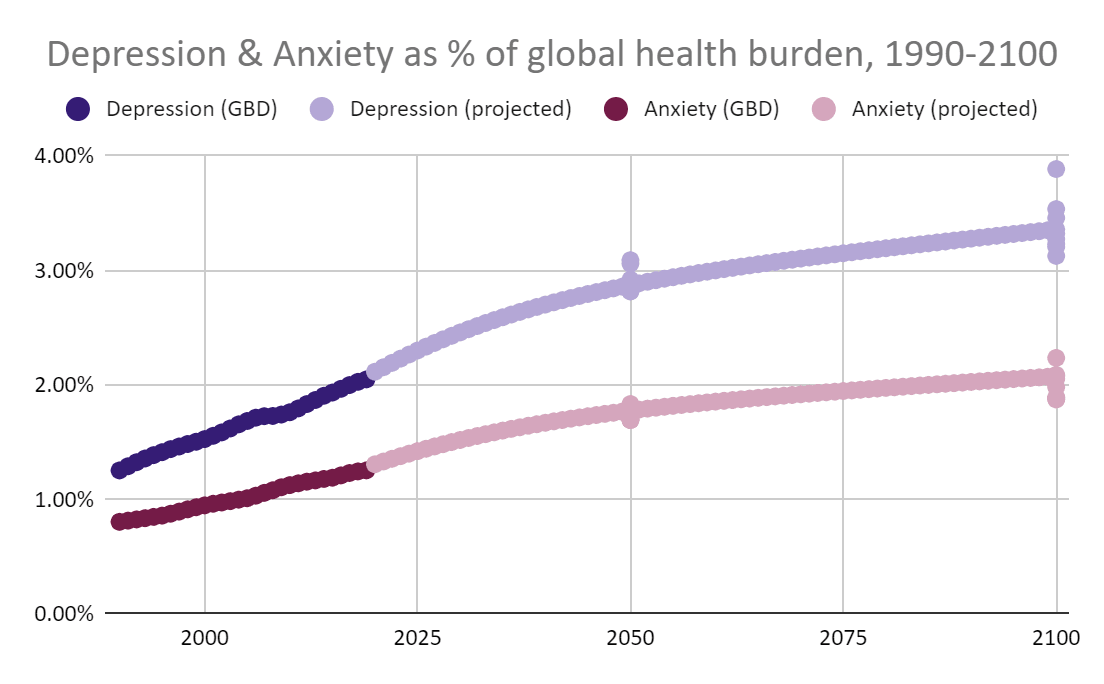
If rapid progress against communicable diseases and malnutrition continues, we can expect mental illness to rise up the agenda. We project that depression and anxiety, the most prevalent mental disorders, will increase 50% in relative importance by the end of the century.
The extra points at 2050 and 2100 are the outputs of various linear and exponential models based on 1990-2019 data.
How bad is mental illness?
DALYs, QALYs and WELLBYs are among the units most often used to measure health. But they may not be well-suited for capturing mental illness.
DALY and QALY weightings come from the assessments of the general public, many of whom have never experienced the health state in question. We suspect that because of its “invisibility”, this leads to a relative underweighting of mental illness. Our analysis of how sufferers of depression rate depression suggests that the condition is around 20% more severe than IHME’s DALY weighting.
The WELLBY is derived from individuals’ assessments of their own lives. This may allow us to capture important effects beyond health or quality of life. But it also introduces the potential for response bias that clouds results. The same goes for other survey methods that gauge mental health by checking for symptoms.
Most measures, including the DALY, QALY and WELLBY, are bounded and therefore cannot capture extreme positive and negative states of being. If we believe that extreme suffering is possible and widespread, we probably ought to weigh severe pain, depression and psychosis more heavily than these measures allow.
Comparing mental illness to other illnesses is inherently difficult. We think that converting between measures should be avoided when possible, because of the highly contested assumptions required. Overall, decision-makers should be aware of the limitations of the measures they are using, and should be clear about any philosophical assumptions they are making.
Treatment interventions
In general, we find that the most important consideration for treatment interventions is the cost per person treated. For this reason, and because of the lack of existing mental health provision, LMICs are usually the best target. The weakness of existing mental health infrastructure in these regions means that organizations should be prepared to overcome major logistical challenges.
Task-shifted interpersonal group therapy is a proven way of scaling up mental health provision in LMICs. However, a controversy over StrongMinds exposed key weaknesses in the literature on psychotherapy and its sensitivity to the methods used to account for bias. Furthermore, estimates for the scale of household spillover effects and the persistence of benefits, which are crucial to the overall effect, rely on few data points. The internet, smartphones and AI offer the potential to deliver psychotherapy more cheaply and to scale up more easily, although this field is in its early stages.
There are huge gaps in access to antidepressants and pain medication in poor countries. Improving access could be highly effective at reducing suffering, but we suspect that it would be a greater challenge than simply providing medicines. One option is to simply improve health workers’ pain-management by providing targeted training.
As mental health in LMICs increases in importance, we should aim to fail fast and improve quickly. We need better evidence on the full effects of interventions over time and across the community. Ambitious programs that garner useful feedback should be valued highly.
Prevention Interventions
This report devotes more space to prevention interventions than treatment interventions, but this should not be seen as an indication that prevention interventions are more promising overall.
We investigate a number of risk factors associated with a higher risk of mental illness. Overall we are surprised at the widespread acceptance of simple correlational evidence and the lack of evidence for causation. Genetic susceptibility and poverty seem likely to explain some of the correlation observed between, say, alcohol abuse and suicide, but studies often do a poor job at isolating these effects.
Interventions targeting risk factors typically have only a small effect on mental health. Cash transfers appear to have a very modest effect on mental health for the spending required. The effect of contraceptive access on averted perinatal depression is likely to be small. Extremely potent risk factors like intimate partner violence may be an exception to this rule.
When the effect size is small, only very cheap and scalable interventions show promise. Health policy “nudges” like sugar taxes or promoting physical activity may operate efficiently enough to avert a year of depression for tens or hundreds of dollars.
We were surprised by the degree to which many suicides appear to be preventable, especially in societies where suicide is taboo. Advocating for bans on deadly means of suicide could have an outsize impact, even though major progress has already been made on this front. It’s even possible that supplementing drinking water with small amounts of lithium could slash the suicide rate.
Much of our work on preventing mental illness relies on speculation. More research is needed on the counterfactual impact of targeting mental health risk factors.
Intervention BOTECs
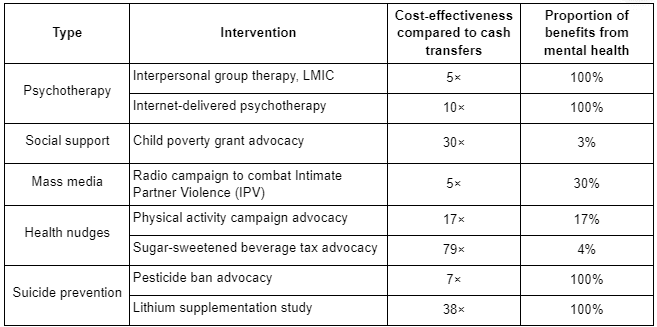
We have constructed BOTECs for the cost-effectiveness of various mental health calculations. Most of the inputs are subjective estimates, and all results should be interpreted with caution. We find that there is generally more uncertainty around policy interventions due to the unknown probability of successfully influencing policy and the unknown scale of the effects. Psychotherapy is a relatively “safe” option, but it is likely to fall short of the best interventions for tackling malaria and other highly preventable diseases.
We hope the calculations can help users determine the most important unknowns in an intervention’s effectiveness. With more context-specific information, the model can be adapted to give more accurate estimates.
Conclusion
Mental illness is a huge problem. We are still refining ways to cost-effectively treat it, and the field of prevention is in its infancy. This means that even the best-understood mental health treatments such as psychotherapy are riskier than the most robust physical health interventions. Mental health work will appeal most to people who prioritize reducing suffering over extending life. Due to the state of the field, we suggest that a premium be placed on interventions that improve our understanding by addressing key questions and filling important gaps in the scientific literature.

Just commenting to say that I endorse this report. I think it contains the forum's very best summary on EA mental health space. Upon first read, there's nothing in there that I object to or that I feel my peers would.
I echo what John Salter said: this is great and it's important to have more of reports like this to elevate the mental health cause area.
Regarding health burden, what's shown here is a significant underreporting. There is strong evidence that poor mental health leads to increased physical health problems. Some sources to consider are the Adverse Childhood Experiences (ACEs) study by the American CDC ( ACEs Aware is a good resource, too), The Loneliness and Isolation report by the US Surgeon General, The Harvard Grant Study, and the Rosteo Study.
Dr David Burns through the feeling great book and feeling good podcast have had a very large positive impact on my mental health for essentially 0 cost on my end. While the feeling good app is still in beta, maybe it's worth reaching out to him (or other mental health app makers) about trialing the app in a low income country. Running a rct may be cheaper in the developing world. If app based interventions work, I'm sure the app creators would be very pleased and I imagine they may be willing to distribute freely in certain regions in exchange for the good publicity.
Thanks for the recommendation! I came across something similar recently: Action for Happiness, which is recommended by Founders' Pledge. I think the theory of change is that people can meaningfully improve their wellbeing by applying some evidence-based changes to their lives. Most who start will probably drop out, but those who persevere will likely benefit. Costs could be kept low by relying on centralised resources, voluntary donations and possibly volunteer labour.
Unfortunately my report didn't explore this avenue for change as I only looked at preventing and mitigating mental illness (+ pain + suicide), but I wish I had done more on simply improving wellbeing.
I would say that although self-help is, on the face of it, basically free, the cost of reaching new people through marketing is likely to be a huge determinant of how cost-effective it is.
You may be interested in this recent meta-analysis on the efficacy of mental health apps. The authors conclude that: "apps have overall small but significant effects on symptoms of depression and generalized anxiety, and that specific features of apps – such as CBT or mood monitoring features and chatbot technology – are associated with larger effect sizes."