Note: This report has been superseded by our subsequent Intermediate Report on Hypertension - please browse that report for our most updated findings.
Summary
Taking into account the expected benefits of eliminating hypertension (i.e. improved health and greater economic output), as well as the tractability of sodium taxation policy advocacy, I find that the marginal expected value of sodium taxation policy advocacy to control hypertension to be 190,927 DALYs per USD 100,000, which is around 300x as cost-effective as giving to a GiveWell top charity.
Key Points
- Importance: This is a strongly important cause, with 1.28 * 1010 DALYs at stake from now to the indefinite future. Around 84% of the burden is health related, while 16% is economic in nature.
- Neglectedness: Whatever governments/charities/businesses are doing to solve this problem (e.g. labelling laws/providing low sodium food in food banks/developing new hypertension drugs) may be making a difference, since age-standardized DALYs lost are falling, but (a) attribution is hard, and structural factors (e.g. more educated populations eating and exercising better, or economic development expanding access to healthcare) will also be behind the decline; and (b) all this is insufficient all the same, with population growth and ageing driving an increase in DALYs lost over time for the coming decades.
- Tractability: A moderately tractable solution in the form of sodium taxes is available. This is highly effective if and when implemented, but there is of course considerably uncertainty as to whether advocacy for taxes on food – which are highly unpopular – can succeed.
Further Discussion
- This is a highly promising cause area that CEARCH will be conducting deeper research into, but it is important to note that early stage CEAs tend to be overoptimistic, and it is likely that this initial x300 GiveWell estimate will be revised downwards after more research and greater scrutiny, possibly extremely substantially (e.g. a one or two magnitude downgrade in cost-effectiveness).
- DALYs lost to hypertension have grown tremendously (43.5%) from 1990 to 2015, and it is certainly not just a rich world problem – over that same period, DALYs lost to hypertension in LMICs exploded (45% increase in high-middle income countries, 72% increase in middle income countries, 94% in low-middle income countries, and 86% in low income countries); and of the large countries, Bangladesh notably saw a fairly staggering near-tripling of DALYs lost.
- Growth in DALYs lost is driven not just by population growth and ageing, but also by urbanization and corresponding lifestyle changes (e.g. excessive dietary sodium, stress, sedentary lifestyle etc).
- Note that the analysis here does not model income effects from the tax (i.e. reduced purchasing power causing less consumption of healthy food) or substitution effects, whether positive (e.g. reducing sugar and fat consumption from food – such as junk food – that is high in not just salt but also sugar and fat) or negative (i.e. causing people to switch to low-salt high-sugar food or drinks); the analysis here also does not model the impact of industry reformulating food products in response to a sodium tax. My sense is that these balance out to some extent, but it is very hard to say.
- There is extremely high uncertainty over the calculations over how the problem will grow or shrink in the coming decades. This is certainly an area where expert advice and expert epidemiological modelling would be extremely valuable, and is something that CEARCH will pursue at deeper research stages.
- We underestimate the economic burden insofar as it focuses on the burden from hypertension (i.e. SBP of > 140 mm Hg) even though high systolic blood pressure (i.e. SBP of > 110-115 mm Hg) has adverse health consequences and presumably negative economic effects as well.
- The estimate of the degree to which an average 1 mg reduction in sodium consumption reduces incidence of high systolic blood pressure in a single country and hence the global disease burden of hypertension, relies on an extremely long and complicated chain of calculations – there is hence a high degree of uncertainty here.
- I do not model the cost of the tax in terms of reduced freedom of choice, because the disvalue of reduced freedom typically ends up as a rounding error in CEAs of policy interventions – except in cases where we're considering banning consumption altogether; there freedom of choice tends to outweigh the remaining marginal health benefits not yet already captured by high taxes.
- Further, I do not model the cost of the tax in terms of reduced pleasure/subjective well-being from less eating of saltier (and presumably tastier) food – on the presumption that excessive consumption of sodium leads to desensitization, while a reduction reverses such desensitization (parallel to how fruits taste sweeter after artificial sugars are cut out from a diet). Hence, there is no real counterfactual loss in subjective well-being expected from the sodium tax and the consequent dietary changes.
- Intensely promising results are driven by heavily discounting the value of the average government's spending relative to EA funding, but even if this were not the case, the intervention would still be in the range of one magnitude more cost-effective than top GiveWell charities – not particularly surprising, for low-probability but high-impact policy interventions.
- Results are also sensitive to the number of years a charity will be operating in a single country (until it either succeeds or concludes that it has failed).
Expected Benefit: Improved Health from Eliminating Hypertension
The primary expected benefit from eliminating hypertension is improved health, in terms of fewer deaths as well as less disability and suffering. Overall, around 1.08 * 1010 DALYs are at stake here, with this benefit is modelled in the following way.
Moral Weights & Scale: Hypertension is defined as systolic blood pressure of >140 mm Hg, but high systolic blood pressure of even > 110-115 mm Hg is detrimental to health, and the overall expected disease burden for 2023 – using 2019 figures as a baseline and projecting forward using a multivariate regression model – is around 2.43 * 108 DALYs. The modelling will be discussed in greater detail subsequently.
Persistence: The problem of high systolic blood pressure is likely to persist, and eliminating it will bring benefits not just for one year but across multiple years. In terms of how this multi-year benefit is calculated:
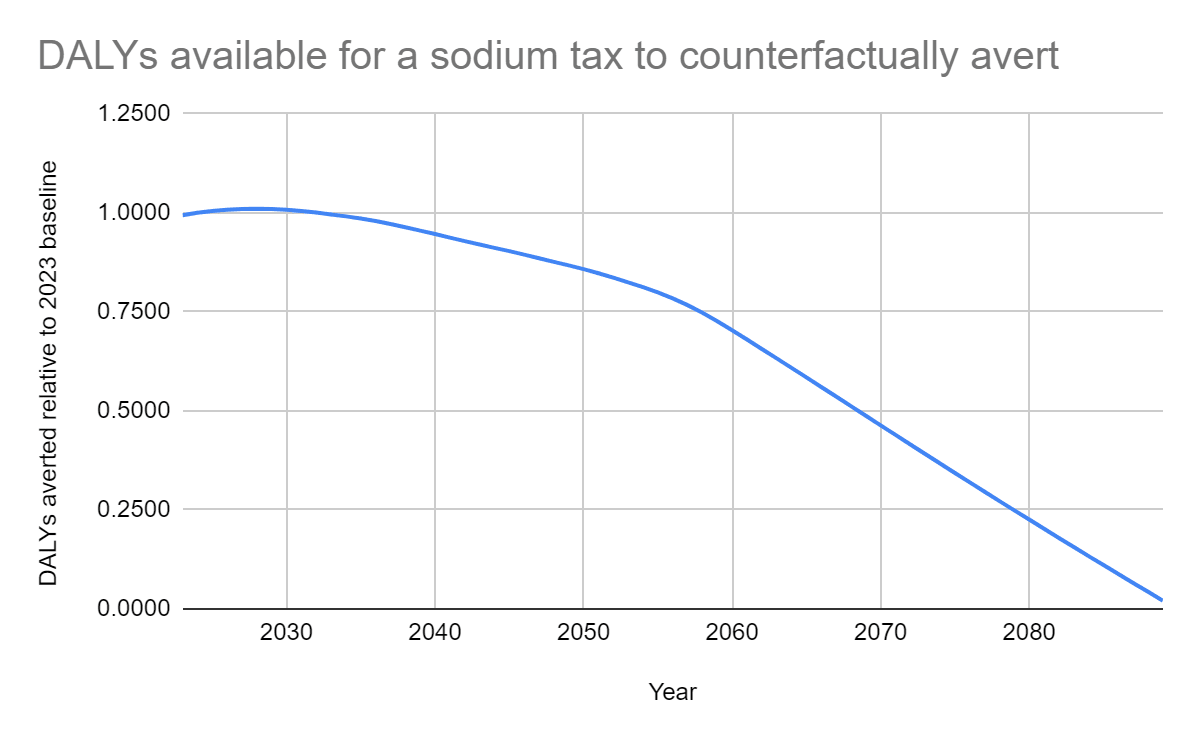
Firstly, I discount for the probability of our solution not persisting (i.e. a sodium tax being reversed). There are few instances of existing taxes on sodium, and the few that exist have not been reversed, yielding a 0% reversal rate – which will be inaccurate, not just because there is a priori at least some chance of reversal, but also because this probability could be fairly high given the unpopularity of food taxes. Instead, I look at the rate of policy reversal on sugary drinks as a proxy of probable reversal on a potential sodium tax, by taking the country-years in which repeal occurred and dividing by the country-years in which the tax existed and repealed could have occurred (whether or not it did). This yields a reversal rate of 0.4% per annum.
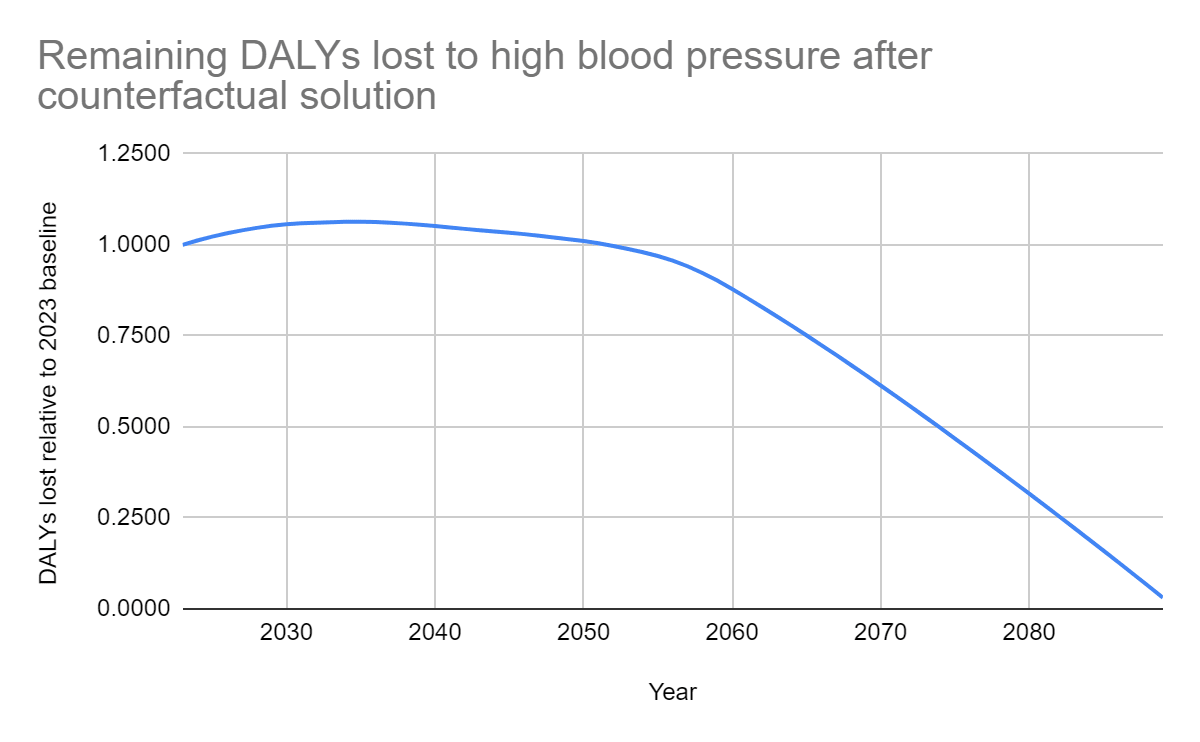
Secondly, I model the proportion of disease burden remaining after being counterfactually solved (i.e. hypertension declining due to the intervention of other actors or else due to structural changes). In fact, unlike most other problems CEARCH has examined, high systolic blood pressure as a problem is likely to grow, at least for some time. To model such growth and the problem subsequently fading away, and on the understanding that total DALYs lost is a function of age-standardized DALYs lost per capita, population size as well as population age, I:
- Regress DALYs from 1990-2019 on age-standardized DALYs lost per capita, population and median age to estimate the relevant linear coefficients.
- Use projected future age-standardized DALYs lost per capita, projected future population, projected future median age and the relevant linear coefficients to project future DALYs lost; and
- Calculate the size of the disease burden for each year from 2023 to 2089 (after which the disease burden finally shrinks to zero) relative to the 2023 baseline.
Conceptually, the role of agents (e.g. governments, charities and businesses) in solving the problem is accounted for via the variable of age-standardized DALYs lost per capita, since anything these agents do to solve the problem (e.g. governments expanding food labelling laws to discourage sodium consumption, or funding access to hypertension drugs; or charities ensuring that the food they distribute via food banks are low in sodium, or providing hypertension treatment in the nonprofit hospitals they run; or businesses doing their part, however little, like food companies reformulating food to appeal to health-conscious consumers, or pharmaceutical companies developing new hypertension drugs to meet market demand), will affect the extent of hypertension in an age-standardized population and the extent to which such hypertension translates to actual death, disability or suffering. To the extent that such efforts by agents to combat the problem is increasingly (or decreasingly) successful over time, that shows up in a decline (or increase) in age-standardized DALYs lost per capita.
Meanwhile, in terms of the role of structural factors – obviously, demographic variables are accounted for through population size and age structure, but cultural and economic factors are also accounted for, through the variable of age-standardized DALYs lost per capita. To the extent that cultural trends affects hypertension DALYs (e.g. as the world becomes increasingly educated, eating/exercise habits improve), and to the extent that economic trends do the same (e.g. as the world gets richer, access to healthcare improves, as does improving technology increases the effectiveness of frontier healthcare treatment for hypertension), that shows up as a decline (or increase) in age-standardized DALYs lost per capita.
The projected growth and eventual decline of DALYS lost due to high blood pressure given counterfactual solution, is shown in Diagram 1.
Diagram 1: Remaining DALYs lost to high blood pressure after counterfactual solution
Thirdly, I discount for the probability of the world being destroyed anyway (i.e. general existential risk discount). Here, I take into account the probability of total nuclear annihilation, since the benefits of saving people from death from hypertension in one year is nullified if they had already died in a previous year. For the exact risk of total nuclear annihilation, I take it to be one magnitude lower than the risk of nuclear war itself, since nuclear war may not kill everyone. For the probability of nuclear war, I use the various estimates on the probability of nuclear war per annum collated by Luisa, but with accidental nuclear war factored in, and then calculate a weighted average that significantly favours the superforecasters. The reason for this is that (a) the estimate of the probability of intentional nuclear war based on historical frequency is likely biased upwards due to historical use being in a MAD-free context; (b) the probability of accidental nuclear war based on historical close calls is highly uncertain due to the difficulty of translating close calls to actual probabilities of eventual launch; and (c) experts are notoriously bad at long-range forecasts, relative to superforecasters. Meanwhile, I do not take into account other existential risks like supervolcano eruption and asteroid impact, since the chances of those occurring at all is very marginal per Denkenberger & Pearce, let alone the chances of such events killing everyone and not just most people. Overall, therefore, I treat the general existential risk discount to be just the risk of nuclear war but adjusted a magnitude down (i.e. 0.07% per annum).
Fourthly, I apply a broad uncertainty discount of 0.1% per annum to take into account the fact that there is a non-zero chance that in the future, the benefits or costs do not persist for factors we do not and cannot identify in the present (e.g. actors directing resources to solve the problem when none are currently doing so).
Overall, by taking the remaining DALYs lost to high blood pressure after counterfactual solution, and discounting each year's DALY burden using the other per annum discounts (i.e. solution reversal discount, existential risk discount, uncertainty discount), the total amount of DALYs available for a sodium tax to counterfactually avert is shown in Diagram 2.
Diagram 2: DALYs available for a sodium tax to counterfactually avert
Value of Outcome: Overall, the raw perpetual value of improved health from eliminating hypertension is 1.08 * 1010 DALYs.
Probability of Occurrence: Unlike longtermist problems, there is no uncertainty as to whether hypertension is a problem – indeed, in 2010, high blood pressure emerged as the leading single risk factor for the overall global burden of disease, surpassing diseases like diarrheal illness and pneumonia. Consequently, I assign a 100% chance to hypertension being an actual problem that harms people.
Expected Value: Hence, the expected value of improved health from eliminating hypertension is 1.08 * 1010 DALYs.
Expected Benefit: Increased Economic Output
Beyond the health benefits, there are also economic benefits to eliminating hypertension. Around 2 * 109 DALYs are at stake here, as calculated in the following manner.
Moral Weights: I take the value of doubling consumption for one person for one year to be 0.21 DALYs. This is calculated as a function of (a) the value of consumption relative to life from GiveWell's IDinsight survey of the community perspective, as adjusted for social desirability bias, and (b) CEARCH's estimate of the value of a full, healthy life in DALY terms. For more details, refer to CEARCH's evaluative framework.
Scale: I start by calculating the economic burden of hypertension relative to annual income per hypertension (i.e. SBP of > 140 mm Hg) sufferer, using three separate estimates to do so.
The first estimate is Wierzejska et al's. I take this estimate of global cost per hypertension sufferer (inclusive of both direct and indirect costs, where direct costs are costs related to treatment and care, while indirect costs are economic costs caused by decreased productivity and reduced labour hours from illness-induced absenteeism and premature deaths); then I divide through by global GDP per capita (using PPP given that is what the authors calculate, and also using the authors' year of calculation); and this yields an estimate of the economic burden of hypertension relative to annual income per hypertension sufferer.
The second estimate is Druss et al's. I take this estimate of US cost per hypertension sufferer, as a function of total costs divided by estimated number of sufferers (itself a function of population prevalence and US population), and divide through by US GDP per capita (using the year of data collection), to estimate the economic burden of hypertension relative to annual income per hypertension sufferer.
The third and final estimate is Cai et al's. I take this estimate of Chinese cost per hypertension sufferer, and divide through by Chinese GDP per capita (using the authors' year of calculation), to estimate the economic burden of hypertension relative to annual income per hypertension sufferer
In terms of how these three estimates of the economic burden of hypertension are weighed, I penalize Druss et al and Cai et al given that they are single country estimates, unlike Wierzejska et al's global, 15-country analysis. This in turn yields the degree of consumption doubling per hypertension sufferer if their hypertension is prevented. And factoring in the global number of hypertension sufferers, we get 213 million doublings in consumption from hypertension being resolved.
Persistence: The same per annum discounts and the same projections of the disease burden (and hence economic burden) over time, as discussed in the previous section, are used here as well.
Value of Outcome: Overall, the raw perpetual value of increased economic output is 2 * 109 DALYs.
Probability of Occurrence: Same probability as before is applied.
Expected Value: All in all, the expected value of increased economic output is 2 * 109 DALYs.
Tractability
To summarize our tractability findings: we can solve 0.00002 of the problem with a USD 137,000 investment into sodium tax policy advocacy, which means the proportion of the problem solved per additional USD 100,000 spent is around 0.0000149.
A sodium tax is chosen over other potential interventions because: (a) as far as dietary factors go, control of sodium intake seems especially important for healthy blood pressure levels; (b) as for other lifestyle interventions (e.g. exercise, reduction in life stress), there does not seem much that external agents can do to change things; and (c) medications, will by their nature be more expensive as an intervention than policy change. In terms of the specific structure of the sodium tax, I consider a tax calibrated to the level of salt content (a type of “nutrient-specific” tax) as these deliver the strongest results in terms of reduced salt intake, largely due to their broad application. And in particular, the tax under consideration is a USD 0.23 (or AUD 0.3) per gram tax on sodium in excess of national health authorities' maximum recommended levels, excluding fresh fruits, vegetables, meats and dairy products, as based on what Cobiac et al (2017) modelled - thus avoiding what would be a political nonstarter (i.e. increasing taxes on basic foodstuffs).
In terms of the theory of change:
- Step 1: Lobby a government to implement a tax on sodium
- Step 2: Sodium tax reduces average daily sodium consumption.
- Step 3: The reduction in sodium consumption reduces incidence of high systolic blood pressure in that single country, and hence reduces the global disease burden of hypertension
Step 1: To estimate the probability of successfully lobbying a government to implement a tax on sodium, I take both an outside and inside view.
For the outside view, I consult three reference classes.
The first reference class is a Thai NGO's long-running efforts in advocating for a sodium tax. The Nephrology Society of Thailand and its Thai Low Salt Network campaign seemed to have started pushing for a sodium tax as early as 2015, and it appears that the tax was to be implemented in 2022, before being delayed in view of the weak economy. With the economy projected to grow stronger, with 4.1% GDP growth in 2023 vs 3.1% in 2022, we might expect the tax to be implemented in 2023, though of course there is considerable uncertainty, with this having been planned before and going nowhere. Hence, I assign only a 50% probability that the tax actually takes place in 2023.
The second reference class involves looking at countries that have introduced a sodium tax as a proportion of those that have a national salt reduction strategy. I take the number of governments that have implemented a tax on sodium, and divide by the number of governments trying to reduce salt consumption; the latter indicates intra-government efforts to control salt, as a proxy for external efforts.
The third reference class is the probability of success for tobacco taxation lobbying efforts. The data here, as collected by Charity Entrepreneurship, is fairly comprehensive, and is relevant to the extent that this is another health policy intervention that involves lobbying governments to introduce or raise taxes on a consumption good.
In terms of weighing the various reference classes to produce an average outside view estimate, it is important to note that all the reference classes have their flaws. The Thai NGO case study focuses on a single country and is hence potentially unrepresentative if there are country-specific factors that bias the estimates (e.g. political conditions are reasonably favourable towards the tax, which is why advocates managed to get it seriously considered and the government seems about to implement it). Meanwhile, the base rate analysis (i.e. sodium taxes introduced as a proportion of all national salt reduction strategies) is flawed because intra-government lobbying is not especially representative of external lobbying efforts - it skips the first step in any policy advocacy theory of change (i.e. securing internal champions for your position). Finally, for the tobacco taxation case study analysis – obviously, there is unrepresentativeness insofar as this is not about a sodium tax at all, and indeed, since tobacco is not seen as a luxury (and is not something literally everyone consumes), the success rate here likely overstates the probable success rate for equivalent lobbying in the salt case. Overall, these flaws balance out, and I weigh the three reference classes equally – yielding a probability of advocacy success of 12%.
For the inside view, I reason as follows. The fact that a salt tax polls at around 42.2% in Ireland and that Tonga has imposed taxes on unhealthy food suggests that successfully advocating for a sodium tax is not extremely improbable (i.e. <=10%). That said, the tax polling underwater and people raising concerns about the impact of such taxes on the poor suggests that successful advocacy is still fairly improbable, and I assign about a 17% chance that advocacy efforts are successful.
Overall, aggregating the outside and inside views, and giving more weight to the former given that the latter is subject to the usual worries about inferential uncertainty, this yields about a 13% chance of advocacy success.
Step 2: I rely on an external empirical estimate to calculate the degree to which the sodium tax reduces average daily sodium consumption in mg. In particular, (a) Cobiac et al's (2017) modelling study shows that an A$ 0.30/g tax on sodium in excess of Australian maximum recommended levels, excluding fresh fruits, vegetables, meats and dairy products, reduced salt consumption by 67mg/day, while (b) Waterlander et al's (2019) experimental study shows that a NZ$ 0.02/100mg and NZ$ 0.04/100 mg tax lead to a 10.7g mean decrease in salt purchased weekly for a household (as averaged across both modelled taxes). To translate the latter into daily reduction in sodium consumption per person, I divide by the average NZ household size of 2.65, then divide by 7 days, and then factor out the 31.9% of food that is purchased but not subsequently eaten. The Cobiac et al (2017) study has the flaw of inferential uncertainty, but the Waterlander et al (2019) study have the flaws of laboratory behaviour not necessarily translating to the real world, serious inferential uncertainty over translating reduced weekly household purchase of sodium in food to actual reduction in daily sodium consumption per person, and concerns over external validity (if the evaluated sodium tax is on sodium in excess of recommended levels while excluding conventionally healthy food) – hence, I penalize the latter by three magnitudes. Overall, I estimate that the sodium tax in question (USD 0.23/AUD 0.3 per gram of sodium) will reduce sodium consumption by 67.33 mg per day.
Step 3: To estimate the degree to which an average 1 mg reduction in sodium consumption reduces incidence of high systolic blood pressure in a single country and hence the global disease burden of hypertension, I rely on a baseline empirical estimate and an accompanying long chain of calculations. He et al (2000) found that a low sodium diet where urinary sodium excretion decreased by 33.3 mmol/24h saw a reduction of cumulative incidence of hypertension from 9.76% to 6.06%. With sodium having an atomic weight of 22.98977 g/mol, this means urinary sodium excretion decreased by 0.7655593 g/24h. 93% of dietary sodium is excreted by urine, so this means that the associated dietary reduction in sodium consumption was 0.8231821 g/24h. Meanwhile, the associated reduction in hypertension from baseline rates is given as 9.76% less 6.06% (i.e. 3.7%) divided by 9.76%, which is 37.91%. Taking the reduction in sodium consumption and the associated reduction in hypertension from baseline rates, this yields a reduction in hypertension from baseline rates of 0.0004605 per 1 mg reduction of daily sodium consumption, in the country where a sodium tax is advocated for and subsequently implemented. Taking that country to be average in population size (i.e. the global population divided by 193 countries), and assuming that reduction in hypertension and high systolic blood pressure not amounting to hypertension is proportional to each other, this yields the fraction of the total problem plaguing the global population, as solved by a 1 mg reduction in sodium consumption in a single country, to be 0.000002.
Overall, the proportion of disease reduction from sodium tax policy advocacy to control hypertension – as a function of (a) the probability of success in persuading a government to pass a tax on sodium, (b) a sodium tax reducing sodium consumption in a country, and (c) reduced sodium consumption in a single country reducing the incidence of high systolic blood pressure in that country and hence the global disease burden of hypertension – is ultimately 0.00002.
Meanwhile, on the costing side, we have to be concerned with both the cost of advocacy (for a nonprofit working on the matter) and the cost of regulation (for the government).
To estimate the cost of advocacy, I take both an outside and inside view. For the outside view, I look at World Action on Salt, Sugar and Health (WASSH), which appears to be a decently successful and well-networked NGO working on salt (and sugar) reduction, and take its annual income in FY 2020-21 in GBP and multiply it by the average 2020 GBP-USD exchange rate. Moreover, I assess that around 1 year of operations is a reasonable timeframe for the charity to lobby/prepare supporting research reports on the health and economics benefits of the tax/do public polling to show public support/construct a coalition of NGOs and advocates in support and hence succeed (in which case it can pivot to a different country) or judge that policymakers are just not receptive and that its efforts have failed (in which case it can pivot or else shutdown).
For the inside view – my sense is that this is doable by a 2 person EA charity in the style of Charity Entrepreneurship incubatees. I assume funding of around USD 50,000 per team member per annum, in line with past CE incubatee expenditures (covering not just salaries but other costs like office rental, lobbying expenditures etc), and again assume 1 year of operations, for reasons aforementioned.
In aggregating the outside and inside views of advocacy costs, I use equal weightage – while the inside view is subject to the usual worries over inferential uncertainties, an EA or EA-identified organization will almost certainly be more cost-effective than WASSH. Overall, this yields an expected cost of USD 123,000 for advocacy in a single country.
As for the cost of regulation – per Cobiac et al (2017), the cost of implementing new taxation and subsidy interventions for foods in Australia is upfront and about AUD 22 million per a 2009 estimate, in 2010 dollars, which translates to a one-time regulatory cost of around USD 0.93 per person given the size of the Australian population in 2009 as well as the exchange rate in 2010. Then I factor in the population size of the average country (in which the intervention will occur), and discount for both the probability that advocacy succeeds (such that the regulatory cost is incurred) as well as the lower counterfactual cost of the average government's spending relative to EA funding going to top GiveWell charities or similar. This is a function of diminishing marginal utility of income, higher average global mean GDP per capita relative to the poor country average, and the top GiveWell health charity's cost-effectiveness relative to just giving cash to poor people, correcting for GiveWell's undervaluation of life vs income. Overall, this yields an expected cost of around USD 14,000 for government regulatory costs.
Put together, the total cost of the intervention will be around USD 137,000.
Consequently, the proportion of the problem solved per additional USD 100,000 spent is around 0.0000149.
Marginal Expected Value of Sodium Taxation Policy Advocacy to Control Hypertension
All in all, the marginal expected value of sodium taxation policy advocacy to control hypertension is 190,927 DALYs per USD 100,000 spent, making this around 300x as cost-effective as a GiveWell top charity.

Thanks for sharing this report! Happy to see more global health content on the forum.
Two quick questions on skimming it:
i) "I assess that around 1 year of operations is a reasonable timeframe for the charity to lobby/prepare supporting research reports on the health and economics benefits of the tax/do public polling to show public support/construct a coalition of NGOs and advocates in support and hence succeed", and
ii) "my sense is that this is doable by a 2 person EA charity in the style of Charity Entrepreneurship incubatees".
I wonder whether you'd be happy to elaborate on these assessments / how you got to these figures, as both seem optimistic to me (though perhaps I'm too cynical).
Thanks again for doing this work!
(commenting in personal capacity etc)
2.43E8 * 5 = 1.215E9
Hi Bruce, thanks for the comments!
On (1): Will definitely be looking to examine the counterfactual policy passage issue more explicitly, in deeper research rounds - but one view is that this is already automatically factored in by any analysis (like the rough one here) of how age-standardized DALYs lost per capita will evolve in the future based on past trends (since any chance in sodium consumption due to policy reasons will show up in both prevalence/severity of hypertension and hence in these age-standardized DALYs).
Any advice on how counterfactual policy passage should be incorporated would be welcome! The way I've done it in the past (and what the way CE does it, I believe) is case study analysis (look at past instances, and calculate country-years of policy passage against total country-years, or something like that), but it's not always wholly satisfactory.
On (2): You're right that this may be too optimistic! My assessment here is based partly on my understanding of the work of CE policy charities (LEEP/PEN/Good Policies), researching and planning out a potential tobacco taxation charity in the recent CE incubation programme (went with CEARCH in the end), and also my past work in government/policy consulting. I have moderate confidence in the view that conditional on there being interest from policymakers, you can work your way up to cabinet ministers within a year in a LMIC and get a yes/no answer by then. I also have high confidence in the view that if the government is not interested, you get the feedback from lower level civil servants long before that, allowing you to pivot accordingly. All this is premised on a high willingness to ignore sunk costs and pivot quickly, and excludes implementation time (folding that into the next year of operations, as you juggle both advising the persuaded government and lobbying the next country)
I'll recalibrate this as I get more expert advice (and also update on the more recent work of CE policy charities, including Mathias Bonde's aid policy organization).
No worries! I'll DM ya some additional thoughts :)
Thanks again!
Hey Joel, great report- overall, I am also pretty excited about interventions for hypertension. A couple of questions about your report:
A great report- thanks Joel!
Hi Akhil! Hope you're enjoying your new role!
(1) I didn't look at community salt substitution at any real depth. My quick prioritization on tractable solutions (definitely the weakest part of the 5-day shallow research process) was that policy intervention via a tax would be more effective than direct delivery (including providing communities with free salt substitutes). And with GiveWell also less optimistic on this issue, there doesn't seem to be a strong case for re-examination.
(2) Didn't look at the other positive effects - will look to incorporate these in deeper research reports, as well as with the negative side effects (especially on how poorer families are likely to be affected - it's going to be the thorniest part of the political case for sodium taxes)
(3) Good point! Will be looking to re-examine the costing, by talking to experts and orgs (especially WASSH) in the area, especially since the topline cost-effectiveness number is so sensitive to this. I think it's very possible that my view is overly influenced by the implicit understanding that this will be an EA organization running on CE-style leanness, but I was also encouraged by the fact that WASSH didn't have a monster budget or anything.
(4) The Thai Low Salt Network seems to be on the verge of success, and WASSH seemed successful in getting supermarkets to reduce product sodium content, but salt taxes are rare enough, and I don't believe there will be many organizations (unlike for sugar) that have a strong track record here. Will definitely be doing a deeper dive on this - unfortunately, deeper case analysis (let along talking to experts) is just really hard to do within the 1-week shallow research stage
I doubt most claims about sodium causing health problems. High sodium consumption seems quite correlated with dietary choices that have other problems, which makes studying this hard.
See Robin Hanson's comments.
It seems the scientific consensus, and Cochrane reviews/meta-analysis of RCTs(e.g. https://www.bmj.com/content/346/bmj.f1325) are supportive. I wouldn't rule out the possibility that sodium isn't as harmful as health authorities think it is (c.f. the whole fracas over saturated fat vs sugar), but I guess I don't see this as a serious worry or something that demands more research given the current evidence/expert opinion and limited research time.
Thanks for writing this! This is really interesting. I only skimmed, but my basic reaction is that I agree that hypertension is an important problem, but am skeptical about salt taxes as a solution. Here are a few reasons why:
1) I suspect salt taxes are less effective at reducing consumption of the offending agent than other kinds of sin taxes (e.g., sugar, tobacco) for two reasons. First, per the linked article, the taxes have historically been applied to salty foods, like chips, instant noodles, and salted nuts. But I suspect a large percentage of the salt people consume comes from the food they cook. Second, it is easier to replace the salt that is taken out of salty foods. You wouldn't buy a sugar-free soda and add sugar to it, but you might well add salt to nuts, instant noodles, and so on. (My parents would buy unsalted microwave popcorn when I was a kid, and I developed workarounds...)
2) This is very speculative, but I worry that salt taxes—which, as you note, will be unpopular—could lead to broader backlash against sin taxes, in much the same way that more draconian masking rules have, perhaps, incited broader backlash against masking. It would be very bad if pushing for salt taxes led to reduced public support for tobacco taxes.
3) Like other commenters, I'm a bit skeptical of the extent to which reducing salt consumption reduces blood pressure. Just looking quickly at this Cochrane review, the drop in systolic blood pressure (SBP) for hypertensive people was 5mm Hg (and only 2mm Hg for normotensive people) with reduced salt consumption. These drops may be statistically significant, but I'm not bowled over by their clinical significance. If a patient with a BP of 150/90 reduced their SBP to 145 by limiting salt consumption, you'd put them on an antihypertensive.
4) I'm perhaps most confused by how quickly antihypertensives are dismissed as an option—
"medications, will by their nature be more expensive as an intervention than policy change." My understanding is that the substantial reductions in cardiovascular mortality seen in the Western world are largely attributable to the use of antihypertensives and statins. Even in the US, you can get a 30-day supply of lisinopril for $3.75, and you'd expect this to reduce the above patient's SBP by 17-23 mm Hg—a 3-4x greater reduction than you'd see with reduced salt consumption.
5) Of course, health care costs much more than just the cost of medications. But if you want a policy solution, I'm inclined to think that a better intervention would involve widespread population BP screening and incentivizing providers to prescribe (and patients to take) antihypertensives. Polypills—which include, e.g., antihypertensives, aspirin, and statins—also look really promising and do more than just reduce hypertension, although pharmaceutical companies have little incentive to make these. So I'd also be eager to see policy solutions aimed at making polypills more widely available.
"Public Health England has estimated that 85% of the salt people ingest is already in food at the point of purchase and consumers only add the other 15% during cooking or at the table."
https://www.theguardian.com/society/2022/jun/21/uk-needs-to-tax-salt-in-the-same-way-it-does-sugar-says-heart-charity
Anecdotally, people add less salt to the food they cook themselves than is added to processed foods in the factory. If this is true, even if people do 'top up' salt levels in their food, they will likely still end up with less salt.
Plus there's salt in all sorts of crazy things like breakfast cereal. If that gets reduced, I don't think people are going to start salting their fruit loops.
Thanks for the feedback!
(1) My understanding is that literal packs/shakers of salt sold in supermarkets would not be exempt from the sodium tax. But that raises more dramatic political problems (e.g. at a $0.3 per mg tax, that increases a 500g packet of salt by 100x), and I presume the per mg tax on literal raw salt would have to be far lower. In general, I do agree that substitution with home food is a worry, though there will also be frictions (i.e. not perfect substitutes because of the social element, time needed to cook, etc).
(2) I'm not sure if this is a significant concern - it depends on your frame of reference, and one could easily argue the opposite (e.g. more aggressive sin taxes normalizes them/shifts the overton window, so even if the extreme version gets rejected, people see the more conventional ones like on tobacco and alcohol as reasonable by comparison). In general, I'm not sure if we have strong reason to believe one way or another.
(3) I think I'm fairly deferential to the scientific consensus in this area, which seems strong - it's something I'll definitely look more closely into via expert intervews.
(4) & (5) Generally, direct delivery (whether of medication or general checkups/treatments) is a lot more expensive due to (a) actually requiring ongoing resources, and (b) counterfactual costliness, for an EA charity. I agree that they could be promising, but in the context of a shallow review I made the call to focus on what seemed to be the most impactful solution - I could be wrong!
Thanks - this is super interesting and I agree that hypertension is a promising cause area - and that taxes on unhealthy foods may be a promising intervention.
I agree with your assessment that this is an area of uncertainty. In particular, I think we need to be careful about assuming linear effects on BP and burden of disease based on a very small change in daily sodium intake. You've thought deeply about this problem, so would be keen to hear your thoughts on what I've sketched out below.
You estimated that a tax would reduce sodium consumption by 67 mg per day; a meta-analyses suggests that reducing dietary salt by a mean of 4.4 g per day leads to a mean reduction of systolic BP of 4.18 mm Hg. There was a bigger drop (5.39 mm Hg) in hypertensive people. [Note: my best guess is that your estimate of sodium reduction is for molecular sodium whereas these numbers are for salt - NaCl - 4.4 g of NaCl would be about 1.7 g of Na.] Based on this, I would say it's very generous to assume any more than 0.5 mm Hg average reduction in systolic BP from 67 mg less sodium per day. 0.5 mm Hg is well within measurement error. This may be a case where a very small effect multiplied by a huge number of people still has a huge effect, but I think more evidence would be helpful. In particular, can we find evidence that:
Maybe deriving additional estimates of the health impacts of -67 mg/day salt intake, using different reference classes, could reduce this uncertainty.
Agreed that the linear vs non-linear issue is a major outstanding issue. My rough sense now is that you capture more of the benefits at higher levels of blood pressure (less so at lower levels/for healthier people) - so diminishing returns - but in general I don't have a good answer and it's something I'll have to get a better sense of via expert interviews.
Couple things (I've only skimmed the post):
(I have more questions like this but I'll leave just these three for now.)
(1) & (2) The Cochrane reviews/GBD results (e.g. https://www.bmj.com/content/346/bmj.f1325 on sodium/hypertension and https://jamanetwork.com/journals/jama/fullarticle/2596292 on hypertension/DALYs) and the scientific consensus more generally seems fairly compelling to be, and while I wouldn't rule out all this being wrong (e.g. the saturated fat issue), it seems fairly reasonable/prudent to deprioritize research into this area of uncertainty relative to others.
(3) Taxation is highly effective, because if affects massive numbers of people are low to no additional counterfactual cost. CEAs that I've run myself (or that Charity Entrepreneurship has done) on tobacco/alcohol taxation, plus the extremely strong underlying epidemiological/economic research on the price elasticity of demand for tobacco/alcohol, all reinforces this point.
I'm fairly sympathetic to the freedom of choice argument. Quick calculations I've done on this area suggest that under fairly plausible moral weights of freedom to smoke/drink etc, (a) it's welfare negative to legally ban alcohol/smoking (even leaving aside the black market effects and assuming these taxes work perfectly, which of course they won't); however (b) aggressive taxes while keeping the product legal generally pass the cost-benefit analysis test. See CEARCH's evaluative framework for our treatment of moral weights for freedom, or examples of BOTECs/CEAs where tax policies are evaluated based on both health and freedom considerations.
oh cool! (Also I'm glad you proactively acknowledge the eg saturated fat)
Also, are there risks to over-reduction in salt intake?
Hmmmm. I'm suspicious is because it doesn't make any sense for anyone to decide what's best for me. (Sure, educate me instead, whatever.) (I'm particularly suspicious of this because of the discourse I've seen around proposed 'meat taxes', typically pedaled by people who think the climate and nutritional (and ethical) effects are far worse than I think they are. So I'm worried about the same thing here.)
Although probably appropriate to ignore at the shallow-analysis level, I think one would need to look into substitution effects very carefully at some point. Specifically, I'm concerned that people might substitute other foods that are reinforcing and pleasurable -- for instance, people may substitute fries for brownies, which would have negative effects on (e.g.) diabetes rates. You could get around this with a general "junk food tax," but the difficult of getting that enacted goes up significantly.
Definitely agreed that more advanced modelling has to take into account substitution into sugar - I believe an empirical study in NZ found substitution into sugar, while others found the fat/salt/sugar correlation in food to be high enough that it's actually benefit. Will take a far closer look at this at the deeper research stages!