Abstract
The 2018 EA Mental Health Survey (whose results are available here) measured the prevalence and effects of mental health problems within the Effective Altruism (EA) community. The 2021 EA Mental Health survey was designed to build upon those results by obtaining more information about the experiences of community members who struggle with mental health problems, rather than serving as another community-wide check of mental health prevalence and effects.
From analysis of 352 responses to the survey, we found that members of the Effective Altruism community experience a range of mental health problems, with depression and anxiety being the most common. How challenging people find it to access mental health care varies, though financial difficulties and stigma do not seem to hold back the majority of respondents from receiving mental health care. Rather, one of the most common obstacles reported was difficulty finding useful information about mental health resources.
People are open to trying a range of mental health interventions, and most people have tried psychotherapy, meditation, and mindfulness techniques. Furthermore, people are generally open to receiving help from a range of different types of mental health interventions, and they’re interested in hearing more about what has and hasn’t worked for other members of the EA community.
Survey Purpose
The 2021 EA Mental Health survey was designed to build upon the results of the 2018 EA Mental Health Survey by obtaining more information on the experiences of community members who struggle with mental health problems, rather than re-measuring the prevalence and effects of mental health problems within the EA community. For this reason, questions that collect data on EA involvement, that differentiate between suspected and formal diagnoses, and that quantify the impact of mental health issues on productivity were not included in the design of this survey. Instead, this survey asked questions that allowed participants to indicate what sort of mental health experiences they could use support with, what accessing mental health care was like for them and what sort of intervention strategies they had tried; there was also space to elaborate on one’s thoughts on mental health care access or mental health resources in general.
Survey Distribution
An initial version of the 2021 EA Mental Survey was distributed between March 31, 2021 and April 10, 2021, with one person completing the survey in its initial form on September 7, 2021. After modification of questions concerning an EA Mental Health database (see section EA Mental Health Database below), this survey was redistributed between November 3, 2021 and December and December 31, 2021 via Slack channels, Facebook groups, and the EA Newsletter. Responses were collected up until January 6, 2022.
When the second distribution of this survey first began, the advertisement of the survey did not at first make it clear that its target population was members of the EA community who are struggling with mental health, rather than the EA community as a whole. Because of this, the data for four survey participants collected prior to making this clear was excluded, as those four participants indicated that they were not struggling with mental health problems.
Participants
Sample size
Between March 31, 2021 and January 6, 2022, 352 people consented to participating in and responded to the EA 2021 Mental Health Survey. However, not everyone responded to every question, and so the sample size varies per question; a note of this with the accurate sample size is provided for each question.
Gender
Of those who provided their gender (n = 330) the majority of people identified as male (n = 168; 50.9%) or female (n = 140; 42.4%) (Table 1). The next most represented gender identity was non-binary (n = 11; 3.3%). Other gender identities represented (at least one survey participant per identity) included agender, genderqueer, questioning, male/dis-oriented, male-presenting, not cis, queer (female presenting and raised), and trans woman (Table 1).
Table 1. Gender representation among the survey participants.
| What is your gender? | Number of people | % of sample (n = 330) |
| Male | 168 | 50.9 |
| Female | 140 | 42.4 |
| Nonbinary | 11 | 3.3 |
| Agender | 3 | 0.9 |
| Genderqueer | 2 | 0.6 |
| Questioning | 1 | 0.3 |
| Male/dis-oriented | 1 | 0.3 |
| Male-presenting | 1 | 0.3 |
| Not cis | 1 | 0.3 |
| Queer, Female raised and presenting | 1 | 0.3 |
| Trans woman | 1 | 0.3 |
Age
The majority of survey participants were 21-30 years of age (n = 215; 62.7%) (Figure 1). The next most represented age groups were 31-40 years of age (n = 88; 25.7%) and under 21 years of age (n = 29; 8.5%) (Figure 1). No one over 60 years of age participated in this survey.

Figure 1. Distribution of age groups in the survey sample.
Country of residence
Most survey participants are residents of either the United States (33.7%) or the United Kingdom (28.2%) (Scotland (n = 1) and England (n = 5) were included in the statistic for the UK). There was also a sizable representation for Germany (6.4%), Canada (4%), and Australia (3.7%). Though five continents were represented in this sample, the sample was still very heavily Western and not very representative of the Global South. For a full list of the countries represented in this sample, see Table 2. In order to ensure the anonymity of survey participants from countries with smaller EA communities, responses from countries represented in <1% of responses were grouped into the category ‘Other’.
Table 2. Survey participants’ countries of residence.
| Which country do you live in? | Number of people | % of sample (n = 326) |
| USA | 110 | 33.7 |
| UK | 92 | 28.2 |
| Other | 26 | 8.0 |
| Germany | 21 | 6.4 |
| Canada | 13 | 4.0 |
| Australia | 12 | 3.7 |
| Ireland | 7 | 2.2 |
| Sweden | 7 | 2.2 |
| Spain | 6 | 1.8 |
| Israel | 5 | 1.5 |
| Switzerland | 5 | 1.5 |
| Finland | 4 | 1.2 |
| France | 4 | 1.2 |
| Netherlands | 4 | 1.2 |
| Norway | 4 | 1.2 |
| Philippines | 4 | 1.2 |
| Don’t want to disclose | 1 | 0.3 |
| North America | 1 | 0.3 |
Race / Ethnicity
The vast majority of the sample was composed of people who identify as white (n = 263; 78.7%; Figure 2). Other ethnic groups represented in the sample included people who identify as Asian (n = 33; 9.9%), mixed race / multi-racial (n = 28; 8.4%), Latino/a/x (n = 5; 1.5%), Middle Eastern (n = 2; 0.6%), African (n = 1; 0.3%), Caribbean (n = 1; 0.3%), and Native American (n = 1; 0.3%) (Figure 2).
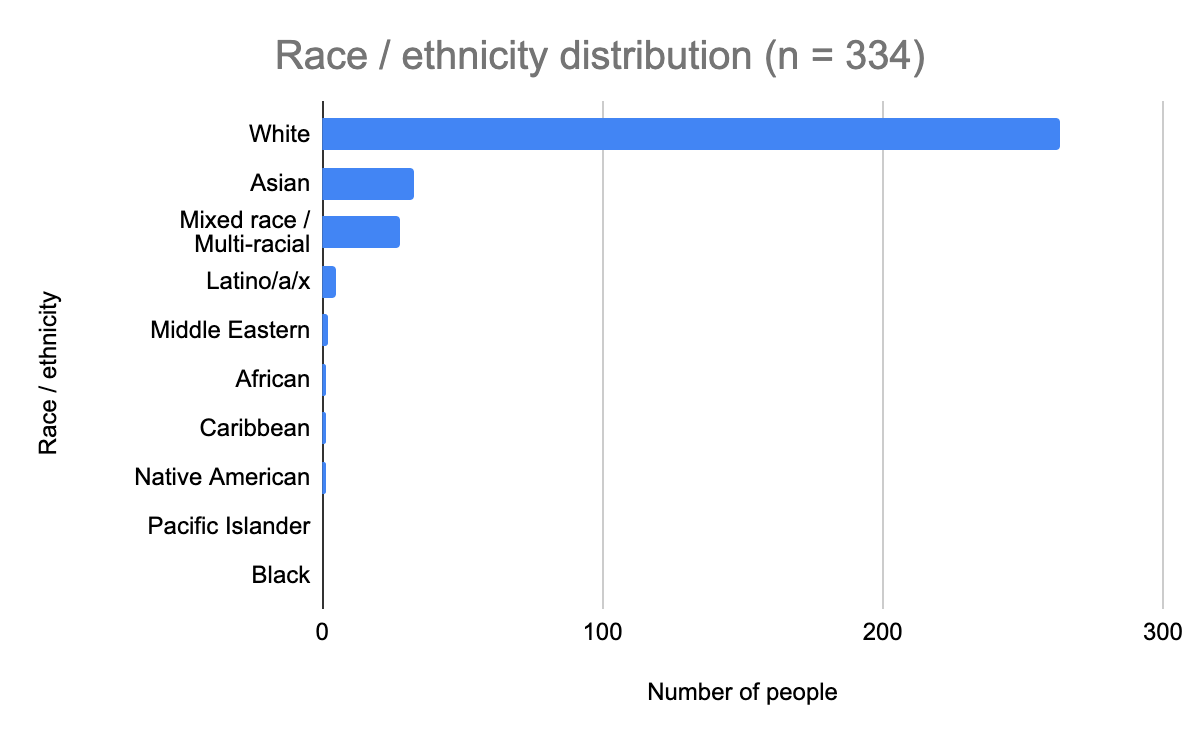
Figure 2. Ethnic groups represented in the sample.
Are the survey demographics representative of the Effect Altruism community?
The sample of community members who participated in this survey is overall representative of the Effective Altruism community, in accord with the most recent surveys on EA demographics (the 2019 EA Survey and then the 2020 EA Survey published on the EA Forum in May 2021), particularly in terms of age, country of residence, and race / ethnicity. See Appendix A for details on the demographics of this survey’s participants.
This sample slightly deviates from being representative in terms of gender representation, as this survey’s sample is more balanced among males and females (50.9% male and 42.4% female, versus approximately 70% male and 27% female in two past EA surveys mentioned) and includes a greater proportion of people who either do not identify with a gender or identify with genders that are neither cis-male nor cis-female (6.7% versus approximately 2-3% in past surveys). However, it isn’t clear whether the gender proportion difference is due to women in EA disproportionately struggling with mental health issues or disproportionately taking the survey.
Results
The survey was split into four parts:
- Mental Health – asked what mental health problems EA community members were experiencing
- Mental Healthcare Access – asked questions about mental health care accessibility
- EA Mental Health Database – asked questions to gauge the popularity of the Mental Health Navigator
- Background – collected demographic information (described in 'Participants' above)
These results will cover each part of the survey, question by question.
Mental Health
This section collected data on mental health problems with which community members struggle by posing the question ‘Which of the following seems closest to what you could use support with? Please check all that apply.’ It is not known whether responses to this question were provided on the basis of self-diagnosis or clinical diagnosis, so there is likely a mix of both. The following options were provided: Depression, Anxiety, Obsessive Compulsive Disorder, Disordered Eating, Addiction, Borderline Personality Disorder, Trauma, Social Difficulties, Attention Deficit Hyperactivity Disorder, Burnout, and Other. The top 10 mental health problems are presented in Table 3.
Table 3. Top 10 mental health problems as of 2021.
| Which of the following seems closest to what you could use support with? Please check all that apply. | # of people | % of sample |
| Anxiety | 212 | 65.8 |
| Depression | 194 | 60.2 |
| Burnout | 158 | 49.1 |
| Social difficulties | 85 | 26.4 |
| Attention deficit hyperactivity disorder (ADHD) | 80 | 24.8 |
| Trauma | 62 | 19.3 |
| Disordered eating | 34 | 10.6 |
| Obsessive compulsive disorder (OCD) | 29 | 9 |
| Addiction | 20 | 6.2 |
| Borderline personality disorder | 13 | 4 |
There was at least one report of each of the following mental health problems (0.3-2.2% of the 322 responses to this question):
- Anger management
- Apathy
- Avoidant personality disorder (AvPD)
- Autism spectrum disorder
- Bipolar disorder
- Brain fog
- Dealing with imposter syndrome / choice paralysis
- Depersonalization / Derealization disorder (DPDR)
- Ecological grief / anxiety
- Ennui
- Excoriation disorder (chronic skin picking or dermatillomania)
- Executive function difficulties
- Existential dread
- Gender dysphoria
- Guilt
- Gut dysbiosis
- Low energy
- Narcissistic personality disorder
- Panic attacks
- Pervasive developmental disorder (PDD)
- Post-traumatic stress disorder (PTSD)
- Psychosis
- Scatterbrained thinking
- Schizophrenia
- Schizoid personality disorder
- Seasonal affective disorder (SAD)
- Setting boundaries
- Sleep-wake disorders
- Suicidality / suicidal thinking
- Supporting family members with mental illness / caregiver fatigue
- Stress
- Trouble focusing
- Unstable mood
The majority of the sample (of the 322 people who answered this question) said they could use help with Depression (65.8%) or Anxiety (60.2%), though there are a range of mental health problems members of the Effective Altruism community could use support with.
Mental Health Care Access
1. How challenging was it to receive the mental healthcare services you needed within the past 12 months?
Of the 346 people who answered this question, 16 found accessing mental healthcare services very easy (4.6%), 55 found it fairly easy (15.9%), 79 found it moderately challenging (22.8%), 69 found it fairly hard (19.9%), and 19 found it very hard (5.5%). 43 people (12.4%) did not need mental health care services in the 12 months preceding participating in the survey, and 65 (18.8%) did not seek out mental health care services but believe they could have benefitted from mental health care. These results are visually depicted in Figure 3.

Figure 3. Results for the question ‘How challenging was it to receive the mental healthcare services you needed within the past 12 months?’ ‘Did not need…’ = ‘I have not needed mental health care services in the past 12 months.’; ‘Did not seek…’ = ‘I did not seek out mental health care services in the past 12 months but believe I could have benefitted from them.”
There was approximately a normal distribution of those who found it very easy to very hard to receive the mental health care services they needed. Of those who did not select an answer on the scale, approximately a fifth of respondents (65 people) did not seek care but believe they could have benefitted from support services. We’ll speculate on what might have held back those who did not seek care from seeking it in the summary section.
2. How challenging is it to find useful information on mental healthcare services?
342 people answered this question. 14 people found it very easy to find useful information on mental health care services (4.1%), 77 people found it fairly easy (22.5%), 110 found it moderately challenging (32.2%), 61 found it fairly hard (17.8%), and 16 found it very hard (4.7%) to find useful information. There were 64 people who did not look for information on mental health care services (18.7%). See Figure 4 for a visual representation of these results.

Figure 4. Results for the question ‘How challenging is it to find useful information on mental healthcare services?’ ‘Did not look’ = ‘I have not looked for information on mental healthcare services.’
There was an approximate normal distribution of those who found it very easy to very hard to find useful information on mental health care services, and about a fifth did not look for mental health care services.
3. Do you experience financial difficulties as a result of mental healthcare?
Of the 342 people who answered this question, 187 said they never experience financial difficulties as a result of mental health care (54.7%), 59 answered ‘rarely’ (17.3%), 67 answered ‘sometimes’ (19.6%), and 29 answered ‘regularly’ (8.5%) (Figure 5).

Figure 5. Results for the question ‘Do you experience financial difficulties as a result of mental healthcare?’
The majority of people who responded to this survey do not experience financial difficulties as a result of mental health care.
4. To what extent does mental health stigma hold you back from receiving the care you need?
Stigma does not appear to be a major barrier to EA community members seeking mental health support, as, of the 344 people answered this question, 142 (41.3%) said mental health stigma does not hold them back at all from receiving the care they need, 144 said stigma somewhat holds them back (41.9%), 37 said it moderately holds them back (10.8%), 19 said it very much so holds them back (5.5%), and 2 said it completely holds them back (0.6%) (Figure 6).

Figure 6. Results for the question ‘To what extent does mental health stigma hold you back from receiving the care you need?’
5. "I am currently receiving the mental healthcare I need."
The fifth question asked survey participants how much they agree with the statement "I am currently receiving the mental healthcare I need." Of the 346 people who responded to this question, 15 strongly disagree (4.3%), 142 disagree (41%), 108 agree (31.2%), and 24 strongly agree (6.9%). 57 people said they do not currently need mental health care (16.5%). These results are visually represented in Figure 7.

Figure 7. Survey respondents’ level of agreement with the statement "I am currently receiving the mental healthcare I need."
6. How satisfied are you with the mental healthcare you've received?
Of the 345 people who answered this question, 72 people have not received mental health care services (20.9%). Of those who answered that they have received mental health care services, 24 were very satisfied with the care they’d received (7%), 143 were fairly satisfied (41.4%), 91 were fairly dissatisfied (26.4%), and 15 were very dissatisfied (4.3%) (Figure 8). This indicates that most people who had received mental health care at the time of taking this survey were satisfied with the care they had received (61.2% of those who had received care).
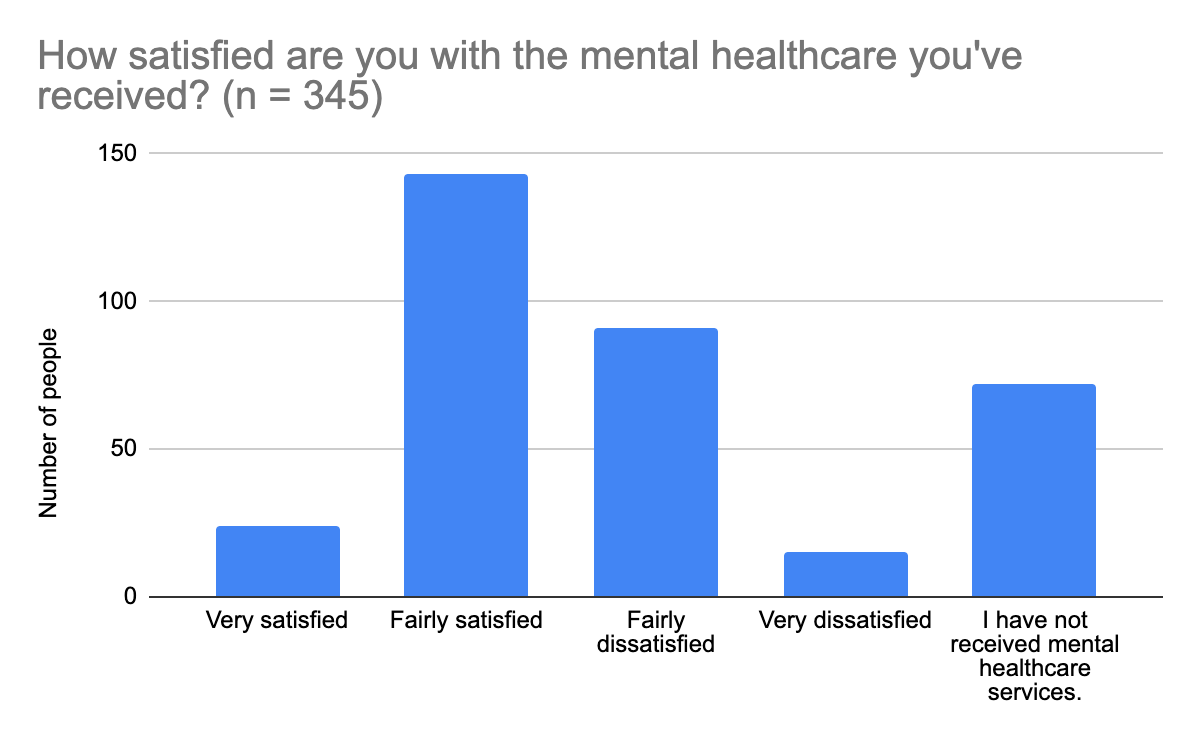
Figure 8. Survey respondents’ level of satisfaction with mental health care received at the time of survey participation.
7. Which of the following have you tried?
This question collected data on what mental health resources people have made use of. Survey participants could choose as many options as they felt were relevant. The following options were provided: Psychotherapy, Prescribed medication, Self-medication, Support groups, Group therapy, Inpatient mental health treatment, Meditation, mindfulness techniques, alternative therapies, Mental health apps, and Other. Meditation, mindfulness techniques, alternative therapies were originally listed as one option together, but I split them up when organizing the results of this question. That way the responses to ‘Other’ could be considered and grouped according to the appropriate option already provided in the survey. Responses to ‘Other’ that did not fit one of the provided options were grouped into new categories. New categories and groupings will be provided below.
Of the 319 people who answered this question, many people have tried Psychotherapy (n = 244; 76.5%), Alternative therapies (n = 228; 71.5%), Meditation (n = 227; 71.2%), and Mindfulness techniques (n = 27; 71.2%). More than a quarter of respondents have also tried Prescribed medication (n = 160; 50.2%), Mental health apps (n = 142; 44.5%), and Self-medication (n = 84; 26.3%). A sizable number of people have tried Group therapy (n = 44; 13.8%), Support groups (including informal student-run groups) (n = 41; 12.9%), and Inpatient mental health treatment (n = 20; 6.3%). Of the options added via ‘Other’ and not recategorized, people have also tried Self-help (n = 10; 3.13%), Counseling (n = 4; 1.25%), Outpatient mental health treatment (n = 3; 0.9%), Peer support (n = 2; 0.63%), Psychedelic substances (n = 2; 0.63%), and nothing at all (n = 2; 0.63%). See Figure 9 for a visual representation of these results.
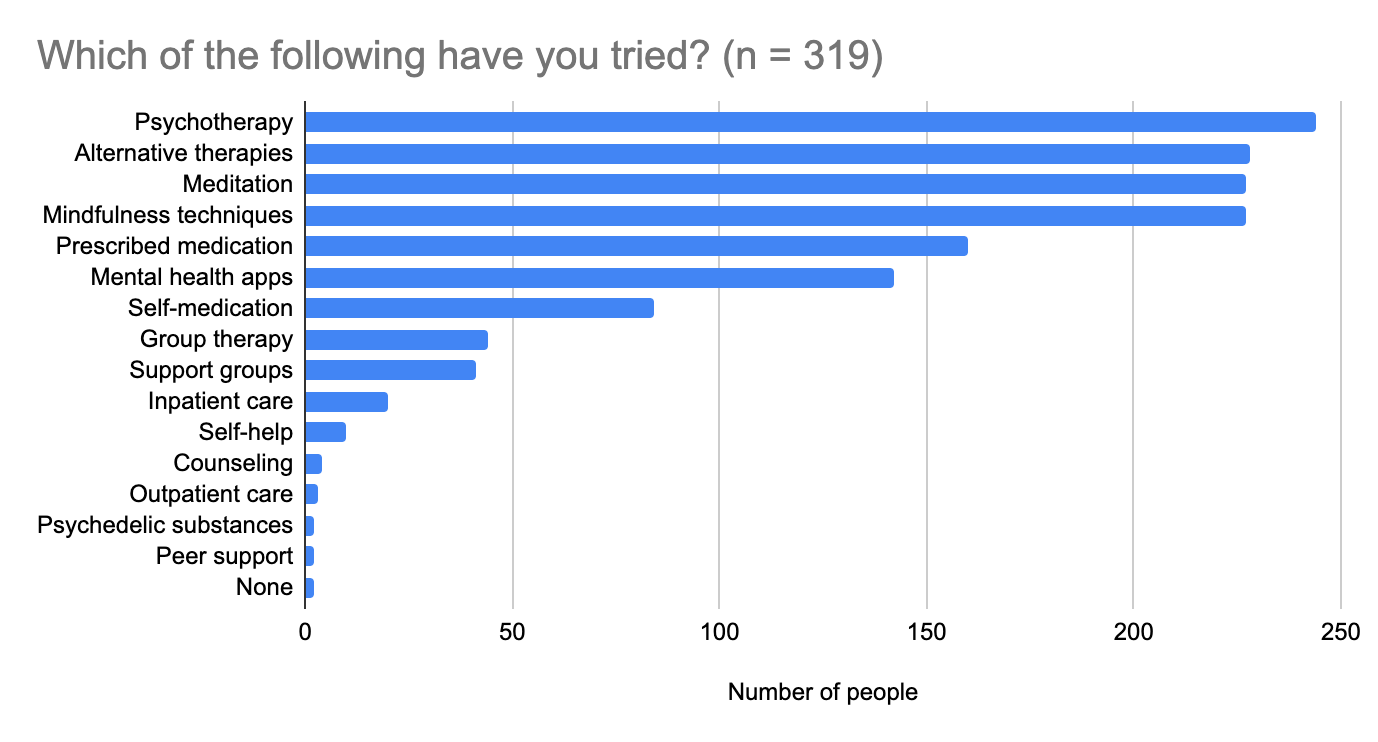
Figure 9. Mental health resources community members have tried and the popularity of those resources among this sample.
Responses to ‘Any other thoughts you'd like to share on mental healthcare access?’ (next question) were sorted into existing categories as indicated below:
Types of psychotherapy tried:
- Acceptance and Commitment Therapy
- Cognitive Behavioral Therapy (CBT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Internet therapy
- Couples’ therapy
Alternative therapies, such as:
- Various modalities from online resources / unlicensed folks, e.g., core transformation or trauma release exercises
Self-help includes:
- Self-therapy and self-practice of techniques
- Workbooks
- Yale's free "Science of Wellbeing" online course on Coursera
- Books
- Employer supported self-care activities
- Discussions with one’s Employee Assistance Program to about strategies for addressing a personal issue during a stressful period at work
Outpatient mental health treatment includes:
- Transcranial magnetic stimulation
Peer support includes:
- Talking to friends
- Informal 1-1 chats with other EAs who also seem hyperactive or have ADHD diagnosed already
In addition to the above, one person was looking for a psychiatrist at the time of participation in this survey.
8. Any other thoughts you'd like to share on mental healthcare access?
73 people answered this question. The answers to this question were of a similar nature to the answers to ‘Any other thoughts you'd like to share on mental health resources?’, which was posed in the EA Mental Health Database section of the survey. For this reason, answers to both questions were pooled and then categorized based on the issue they were addressing. A summary of the responses received is provided in the EA Mental Health Database section below.
9. Summary of this section’s results
To summarize this section, there was approximately a normal distribution of those who found it very easy to very hard to receive the mental health care services they needed. Of those who did not select an answer on the scale, approximately a fifth of respondents (65 people) did not seek care but believe they could have benefitted from support services. Of those who did not seek out mental health care services but believe they could have benefitted from them, financial difficulties and stigma do not appear to be major reasons for not seeking support services, as 53 of the 65 people who did not seek out support said they either never or rarely experienced financial difficulties as a result of mental health care (though perhaps that is simply because help was not sought), and 46 of 65 said stigma either did not hold (16) or somewhat (30) held them back from seeking the care they needed.
Overall, there was an approximate normal distribution of those who found it very easy to very hard to find useful information on mental health care services, and about a fifth did not look for mental health care services.
Most people either agree or disagree with the statement that they’re currently receiving the mental health care they need (i.e., there are no strong thoughts on the statement), though more people disagree with the statement than agree. However, just because people were not currently receiving the care they needed didn’t mean they weren’t satisfied with the care they had received in the past. Most people who had received mental health care at the time of taking this survey were satisfied with the care they had received (61.2% of those who had received care). 20.9% of respondents had not received care.
In terms of intervention strategies, most people have tried psychotherapy (n = 244; 76.5%), alternative therapies (n = 228; 71.5%), meditation (n = 227; 71.2%), and mindfulness techniques (n = 27; 71.2%), though people have also tried a range of other mental health intervention strategies.
EA Mental Health Database
The Mental Health Navigator will use the data in this section as benchmark data for the popularity of the Mental Health Navigator as of 2021. See the sub-section 'Advertisement of the EA Mental Health Navigator through the EA Mental Health Survey?' below for more information.
1. Had you ever heard of the EA Mental Health Navigator Service before participating in this survey?
Of the 308 people who answered this question, 73.4% (n = 226) had not heard of the EA Mental Health Navigator and 26.6% (n = 82) had (Figure 10).
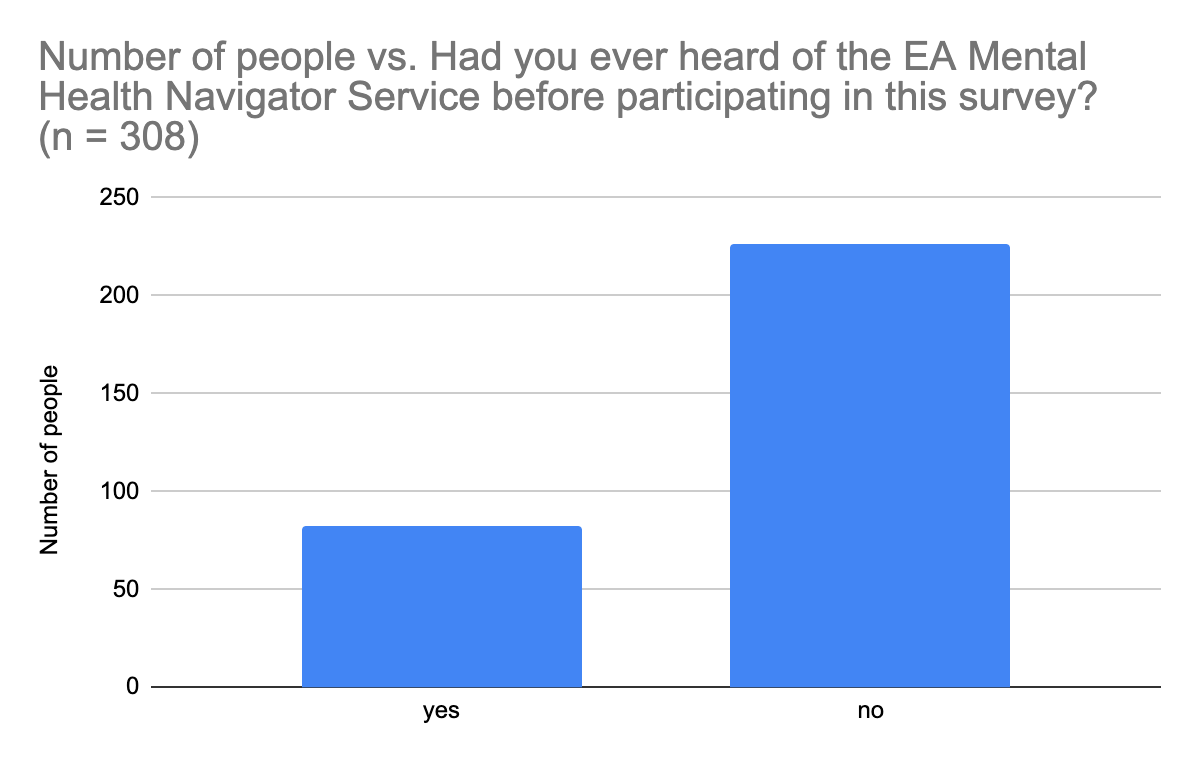
Figure 10. Awareness of the Effective Altruism (EA) Mental Health Navigator among community members as of 2021 (up to January 6, 2022).
2. How likely are you to make use of the EA Mental Health Navigator Service?
Of the 337 people who responded to this question, most people indicated a neutral range of likeliness to make use of the Navigator Service, i.e., they selected values ranging from 3 to 5 on a scale of 1 to 7, with 1 being ‘very unlikely’ and 7 being ‘very likely’ (Figure 11).
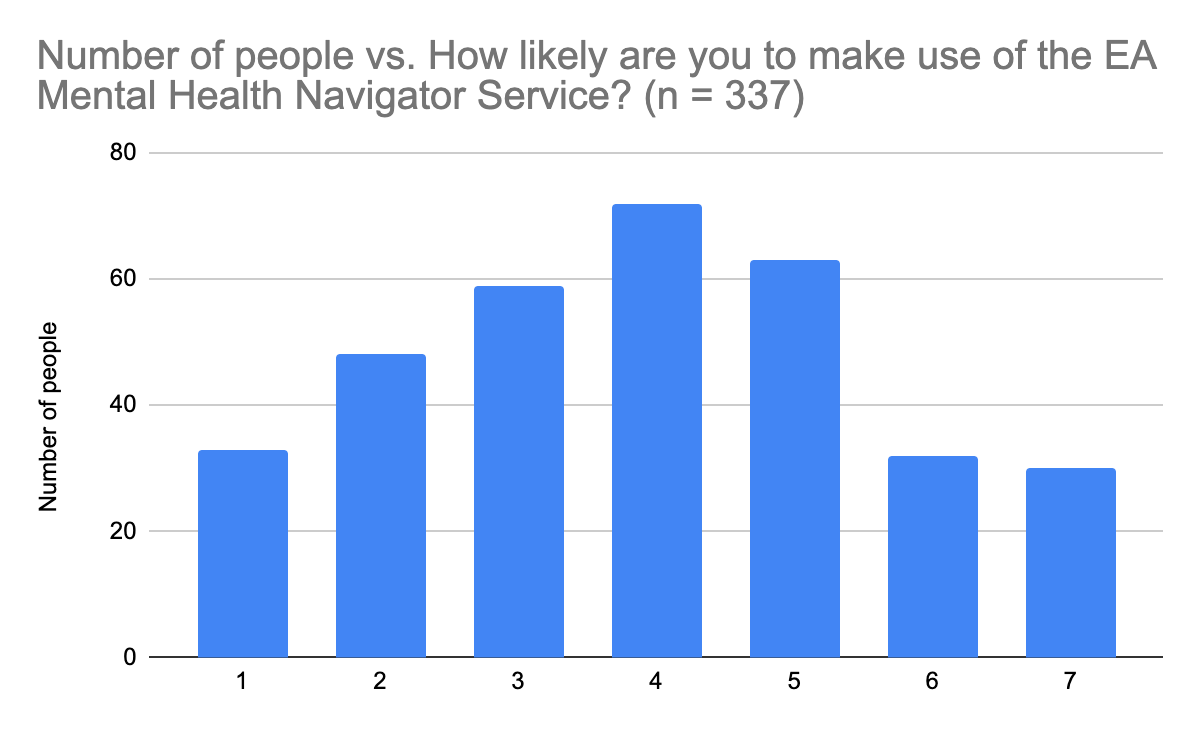
Figure 11. Likelihood of making use of the EA Mental Health Navigator Service. The likelihood scale applied has values ranging from 1 (‘very unlikely to use’) to 7 (‘very likely to use’)
3. How likely are you to recommend the EA Mental Health Navigator to a friend?
Of the 331 people who responded to this question, most people (indicated a neutral range of likeliness to make use of the Navigator Service, i.e., they selected values ranging from 3 to 5 on a scale of 1 to 7, with 1 being ‘very unlikely’ and 7 being ‘very likely’ (Figure 12).
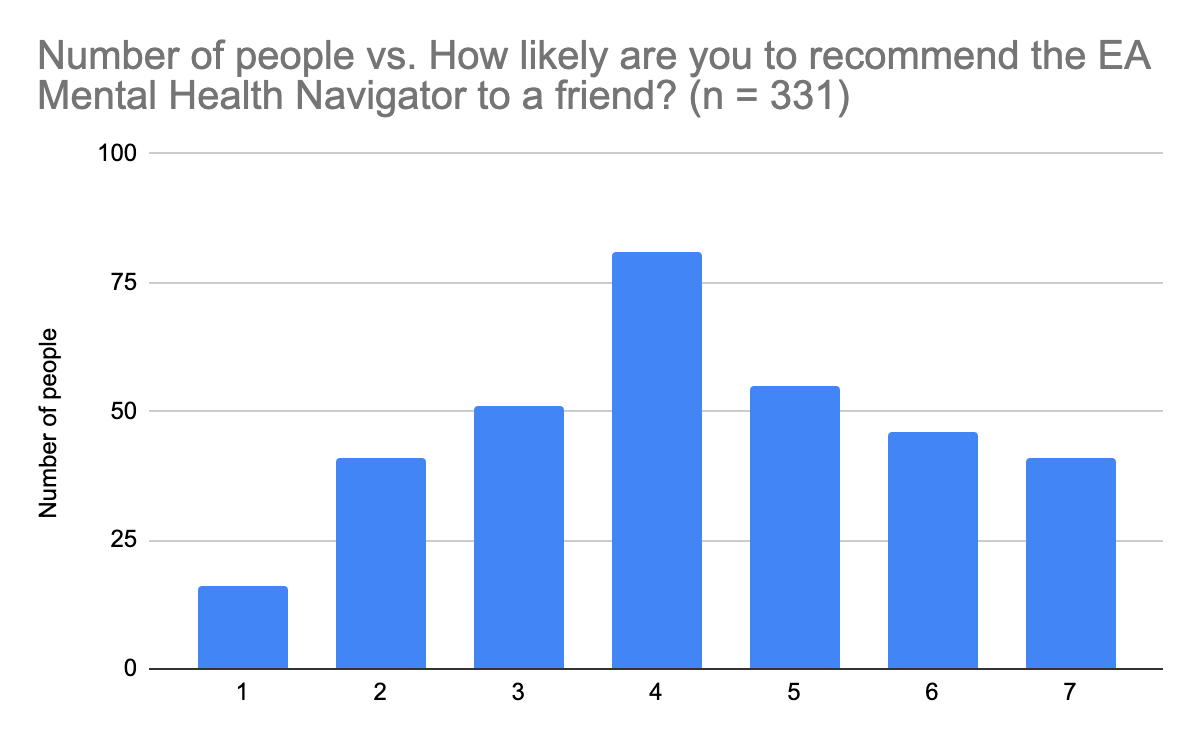
Figure 12. Likelihood of recommending the EA Mental Health Navigator Service to a friend. The likelihood scale applied has values ranging from 1 (‘very unlikely to use’) to 7 (‘very likely to use’).
4. Any other thoughts you'd like to share on mental health resources?
50 people answered this question. Since the answers to this question were of a similar nature to the answers to ‘Any other thoughts you'd like to share on mental healthcare access?’, which was posed in the EA Mental Health Care Access section of the survey, answers to both questions were pooled and then categorized based on the issue they were addressing. A summary of the responses received is provided here, as part of the consent form for this survey stipulated that raw data would be kept confidential.
Comments provided in response to the ‘Any other thoughts’ questions generally fell into the following categories:
- People struggle to navigate mental health care when they’re at a low point
- Thoughts on therapy as a form of mental health support:
- It’s difficult to find a therapist one can trust, especially since therapists have their own approaches to mental health care, one doesn’t always necessarily go in knowing exactly which aspects of one’s health are most important and tractable, and it’s not clear whether or not a therapist is going to be helpful until a considerable amount of time has been invested in sessions with the therapist
- People are interested in what forms of therapy have been helpful to other people in the community
- People are interested in seeing therapists who come recommended by other members of the EA community
- People struggle to find approaches that fit their problems
- There is a lot of information online, but it’s hard to shift through it all to find the good quality resources, especially when one is unsure of what they actually need or what would be most effective given their particular circumstances.
- Some people are able to access care through their employers, but the care provided is not always helpful.
- This is sometimes a result of being misdiagnosed.
- People find it difficult to find therapists who accept the values of Effective Altruism or whom they can trust
- This is particularly the case for those who are interested in seeing EA-aligned therapists, but cannot afford their rates.
- Thoughts on whether an EA-aligned therapist is necessary: some say yes, others no; some say it’s helpful to speak with therapists who are outside of the EA community.
- Expectations of therapy
- People did not have a good understanding of what therapy was like before starting therapy, and so they then learned along the way that therapy is like a course of prescribed medication in that one is expected to reach certain milestones over the course of a given number of sessions.
- Thought therapy would be quick and easy process
- Some see therapy as sessions where therapists are able to use their experience to guide clients through their mental health by asking leading questions.
- Thoughts on meditation as a form of mental health support:
- Meditation (particularly stoic meditation) has been very useful
- People have found meditation apps helpful
- There needs to be a greater awareness of the potentially adverse effects of meditation
- Indication that more information on use of medication or recreational drugs (including psychedelics entactogens) for mental health purposes would be appreciated, so as to be able to make more well-informed decisions about medications and to obtain a more balanced look at the risks associated with using recreational drugs.
- Indication of difficulty finding psychiatric care or prescriptions for preferred medications
- Indication of an interest in learning more about and spreading awareness of symptom patterns
- The mental health resources available are dependent upon one’s country of residence
- Some countries have rather long wait lists for psychotherapy (such as Germany and the UK), and that can be a big problem for people with more acute mental health problems.
- In some countries (such as Sweden), mental health care is affordable and easily accessible, either because the state makes it affordable or because people earn enough to afford the care they need (maybe both are true).
- The mental health care system in the US makes it difficult to find care, especially since social stigma around mental health issues is still pretty strong.
- It can be difficult to receive a diagnosis via public healthcare systems, but if one goes to a private health care provider, that can be expensive (and therefore not affordable for people living on a budget).
- It can be difficult to access mental health care services via the NHS in the UK because it’s difficult to figure out how the NHS works when trying to access specialist care and one may not have mental health symptoms that are considered as severe enough for prompt care (which could then lead worsening of those symptoms until they are very severe and greatly impacting one’s life).
- Publicly available mental health resource information is not kept up-to-date in some countries.
- Receipt of mental health care in one’s native language (not English) is important.
- What holds people back from seeking support:
- Personal stigma
- Public stigma
- Lack of necessary technology (to access online care)
- Lack of availability of long-term providers / providers for chronic conditions
- Insurance (difficult to find the right therapist via one’s insurance plan, either because the right therapist doesn’t accept one’s insurance or because therapists who accept one’s insurance are not currently taking on new patients).
- The monetary cost of mental health care
- Good quality, effective therapists are generally not affordable, especially since they often do not take insurance
- The monetary cost of mental health care is particularly a problem for those who are experiencing financial difficulty, potentially as a result of their mental health problems (such as if they are not able to work for a period of time).
- There is a need for more low-cost apps and services
- The temporal cost of finding good quality mental health care
- Some folks have not found mental health help helpful and / or trustworthy:
- For some this is due to not trusting mental health institutions that have historically not treated people well, such as institutionalizing people against their will
- For some this is due to therapists causing people to question themselves and seriously consider ideas not actually applicable to their particular situations
- Mental health check-ups: Some people are overall doing well and so consider mental health to be low-priority for the time being, but feel it’s good to check-in with a specialist every now and then
- People have a difficult time accessing ADHD services or receiving a diagnosis
- Mental health support options or research suggestions for the Navigator Service
- Feedback for the EA Mental Health Navigator in its 2021 form
Suggested solutions based on the feedback above will be provided below in the section Solutions.
Solutions
Some of the solutions proposed by survey participants and based on the results of this survey can be fairly quickly put into effect as new independent projects or as collaborative efforts between existing EA Mental Health projects. In no particular order of priority or potential effectiveness, these include:
- Creating a blog or other platform for people to be able to (anonymously, if so desired) share their mental health experiences and challenges and connect with each other if they’d like
- Provide more information (and publicize more what we have) on symptoms and patterns of various mental health problems and disorders
- Provide more information on resources to help with the world of dating
- More actively encourage people to recommend psychiatrists
- Provide more science-based information on how to deal with suicidal thoughts
- Provide more information on the importance and effects of nutrition, lifestyle, and other inputs affecting neurobiology on mental health and wellbeing
- More actively encourage people to reach out for support
- Gather information relevant to all of the mental health problems survey respondents mentioned
The Mental Health Navigator is already addressing a few solutions based on these survey results, including:
- Gathering information on mental health resources located outside the US and UK
- Building a country-by-country guide to mental health care access
- Building a guide to different types of therapy, particularly evidence-based and rationalist-friendly therapy
Other solutions proposed will require a bit more planning. These include:
- Creating a fund to support people who cannot afford mental health care, either because the care itself is not affordable or because they can’t afford the technology to access telehealth
- Writing or citing articles that provide more information on medication and recreational drugs as forms of mental health care
- Provision of resources in languages that are not English
- Provide incentives for or compensate good quality therapists for providing lower rates
- Lobby for better mental health care systems and policy changes in countries such as the US
- Lobby for more implementation of more preventative measures worldwide, i.e., systemic changes to social systems
- Invest in mental health research so that diagnoses are more precise and accurate
- A need for more skilled therapists used to working with intelligent, introspective clients
- There is a need for more EA-friendly (not necessarily EA-aligned) therapists who provide a wide range of therapy modalities, especially since CBT does not work for everyone
- Workshops or articles that provide community members with an understanding of how therapy works (e.g., you go for x number of sessions and then are expected to be able to do ___ by yourself afterwards), what makes a good therapist, and how to find a good therapist
- Provide more information on the potentially adverse effects of mental health interventions, such as meditation (one person particularly suggested looking into Willoughby Britton's work and her non-profit, Cheetah House)
- Find ways to encourage and support members of the community who have disabilities, and encourage them to still apply for jobs and roles for which they feel they cannot compete
- Provision of mental health apps for both iOS and Android systems
- Research into autism and females, and what techniques help there to improve mental health
- Provision of articles or coaches to help people with navigating the world of dating
- Set up more support groups
Acknowledgement of what can be improved in future surveys
Nuño Sempere took the time to provide some helpful comments on this survey’s design (unfortunately these comments were only received after the second distribution had begun, and so they were not taken into account at the time of receipt, but they will be considered when designing future iterations of this survey). I will address Nuño’s comments here along with other planned improvements for the next iteration of this survey.
Survey promotion and bias
The demographics of this survey’s participants are representative of the demographics of the EA community as a whole, according to the most recent surveys on EA demographics (the 2019 EA Survey and then the 2020 EA Survey published on the EA Forum in May 2021). However, this survey (and those who work in the EA Mental Health space in general) could have benefitted from more insight from community members residing in locations that do not make up the majority of the sample (i.e., the US and UK). This is particularly true given that the EA Mental Health Navigator aims to provide helpful information and support to all EA community members. Future surveys will therefore do a better job of ensuring that it is not only people with access to Facebook or Slack who are able to access the survey. This will be accomplished through directly emailing future survey links to more EA groups listed on the EA Hub website. This will hopefully reduce the sample bias that was inevitably created by the majority of survey responses coming from residents of the US or the UK.
Furthermore, there was a bias of people who are already interested in mental health or the EA Mental Health Navigator taking this survey, as this survey was designed to gain an understanding of the experiences of those who are currently or have been struggling with mental health. The first question in the EA Mental Health section made this apparent and might have confused respondents not experiencing mental health issues because it did not provide an option relevant to their experiences besides ‘Other’. Should the next survey aim to measure prevalence of mental health problems again alongside gauging mental health experiences, this question will include an answer option such as “I do not currently need mental health support”.
Design the variables such that it is easy to collect and quantitatively analyze the data
This survey was designed to provide more of a qualitative than a quantitative analysis of mental health experiences among EA community members. The open-ended structure of several questions, such as ‘Any other thoughts you'd like to share on mental healthcare access?’ and the option ‘Other: ___’ meant that the data was not grouped as it was collected. These open-ended questions and variables were therefore presented as tables and lists and only subjected to qualitative analysis. It would be interesting to provide all new options obtained from answers to these questions as options in future surveys, so that they are presented as options to the entire community.
Some questions, such as ‘How challenging was it to receive the mental healthcare services you needed within the past 12 months?’ did provide categorical answer options. The results of these questions are primarily depicted via bar graphs that show the frequency of answers.
Inclusion of more options under ‘Which of the following seems closest to what you could use support with?’
Based on the people who added options via ‘Other’ or made suggestions via the ‘Any other thoughts you'd like to share on mental health resources?’ question, the following will be included in future surveys that ask ‘Which of the following seems closest to what you could use support with?’:
Options in a question asking about mental health disorders:
- Avoidant personality disorder (AvPD)
- Autism spectrum disorder / PDD
- Bipolar disorder
- Depersonalization / derealization disorder (DPDR)
- Excoriation (skin picking) disorder
- Narcissistic personality disorder
- Post-traumatic stress disorder (PTSD)
- Schizophrenia
- Schizoid personality disorder
- Seasonal affective disorder (SAD)
- Sleep-wake disorders
Options in a question asking about mental health issues or symptoms (which are not medical disorders themselves):
- Anger management
- Apathy
- Brain fog
- Dealing with imposter syndrome/choice paralysis
- Ecological grief / anxiety
- Ennui
- Executive function difficulties
- Existential dread
- Gender dysphoria
- Guilt
- Disturbances to cognitive and physical function primarily caused by gut dysbiosis
- Low energy
- Panic attacks
- Psychosis
- Scatterbrained thinking
- Setting boundaries
- Suicidality / suicidal ideation
- Supporting family members with mental illness / caregiver fatigue
- Stress
- Trouble focusing
- Unstable mood
Try to distinguish between clinical diagnoses and self-diagnoses
This survey did not specifically ask participants whether they had received official diagnoses for the mental health disorders that they struggle with, so there were likely a mixture of responses from those who had received a diagnosis and those who had self-diagnosed. It could be interesting to make this distinction in future surveys to better understand which mental health disorders EA community members struggle to receive a diagnosis for.
Gauge the severity of mental health problems in the community
This survey did not ask questions to gauge the severity of mental health problems in the community, e.g., how many people meet criteria for clinical depression or how many people experience mild to moderate symptoms of anxiety. Data that gauges the severity of the mental health problems EA community members struggle with could have made this a more informative survey, and it could have made it easier to day what course of actions would be good to take to address the problems people are struggling with. Future surveys will therefore ask questions that gauge the severity of the mental health problems people are struggling with when asking what those problems are.
Directly ask questions about what other topics EAs struggle with
In the first question in this survey, participants were asked to choose from a list of mental health problems that seems closest to what they are struggling with. However, mental health disorders are not the only source of mental health troubles. Some people also struggle with excessive guilt and shame or clinical perfectionism, which are themselves not mental health disorders and therefore not categorized in the Diagnostic and Statistical Manual of Mental Disorders. It would therefore be helpful in future surveys to directly ask community members what other psychological problems or topics they struggle with that they feel contribute to experiencing mental health problems.
Directly ask questions about what types of services people are interested in learning more about
In order for EA Mental Health projects to better provide mental health support, it would also be good to have an idea of what sort of mental health services people would be interested in learning more about. We should therefore ask community members what they’d like to learn about in future posts or surveys.
Investigating universal healthcare
It has been suggested that the survey disambiguates countries with universal healthcare from those without. Future survey iterations will take an interest in evaluating the perceived effectiveness (among EA community members) of mental health services provided by universal healthcare, and so this disambiguation will be made at that time.
Advertisement of the EA Mental Health Navigator through the EA Mental Health Survey?
The section EA Mental Health database seemed to some to serve as an advertisement of the EA Mental Health Navigator. This was not the intention. When the EA Mental Health Navigator first received funding, a survey was planned to gauge the popularity of the Mental Health Navigator as a benchmark against which we could measure its popularity over time. However, the Mental Health Navigator’s project manager was advised to not send around two surveys (the 2021 EA Mental Health Survey and a survey with some questions about the EA Mental Health Navigator) at the same time, and so the key questions necessary to obtaining baseline data from the start of the Mental Health Navigator’s funding were included in the 2021 EA Mental Health Survey. This practice of combining two surveys into one may very well be repeated in the future, particularly if the timing of obtaining metrics of community-wide mental health once again coincides with the timing of measuring awareness of the Navigator Service. However, we will try to avoid combining surveys with two separate purposes in the future by spacing their distributions at least six months apart.
Ask questions about other EA-aligned mental health resources
It was also suggested that this survey include questions about the popularity of other EA-aligned mental health resources, including the EA Off-Road project and the Lorien Psychiatry Database, which provides an overview of different mental health conditions, medications, supplements, and lifestyle suggestions. This is something we plan to do in the future. At the time of distributing the survey, there was not a great awareness of what EA mental health projects were out there, and some new ones were coming into existence. Over the last couple of months, an effort has been made to collect information on what projects exist within the EA Mental Health space and create a platform for people involved in leading or managing those projects to communicate and collaborate with each other; see the footnote below for more information.[1]
Acknowledgements
A big thank you to everyone who participated in the 2021 EA Mental Health Survey! The information you provided will help us to improve the Mental Health Navigator and has already helped several members of the EA Mental Health community think about how we can best help and support a range of community members, from those who are not in immediate distress and would like to improve their mental health to those who are experiencing a crisis and need immediate support.
Author Contributions
Danica Wilbanks, Damon Sasi, Gavin Leech, Ewelina Tur, Gina Hafez, and Thomas Blank designed this survey and Danica began its distribution to the wider EA community in March 2021. Nuño Sempere provided feedback on survey design. Emily Jennings contributed questions concerning the EA Mental Health Navigator, continued distributing the survey in November 2021, and wrote up and posted the results online. Ben Williamson, Ewelina Tur, and Danica Wilbanks kindly provided reviews of the draft of these results before its publication on this forum.
Data Availability Statement
The anonymized data generated and analyzed (with the exception of responses to open-ended questions) are available upon request to the EA Mental Health Navigator at ea.mh.navigator@gmail.com for those who might wish to do follow-up analyses.
Feedback and Comments
Feel free to provide constructive comments and suggestions for the survey design and analysis in the comments below. Should future iterations of this survey be planned, your comments and suggestions will be carefully considered. If you feel more comfortable sending your suggestions or comments by email, feel free to send them to the Mental Health Navigator project manager at ea.mh.navigator@gmail.com.
- ^
A LinkedIn group has been created for people managing mental health projects funded by the Effective Altruism community to have a space to collaborate and communicate with each other about their projects and ideas. Please reach out to Ben Williamson or Emily Jennings if you are currently managing a mental health project and would like to join the group!

So as you discuss, this survey suffers from selection bias. At the time, I suggested[1] looking at SlateStarCodex results instead, filtering by self-reported EA affiliation . I can't find the results for 2021 or 2022, but using results from 2020:
returns
Plotting this:
Code to replicate this here, source for the data here[2]. There are other things one could look at, like whether self-assessed EAs are more likely to be mentally ill, or whether this is mediated by income, student status, etc.
This point was originally suggested by David Moss in the first iteration of the survey; I just remembered.
I downloaded the .xlsx data and converted it to a csv, because the csv data doesn't seem to be available.
I'd love to see a deeper inquiry into which problems of EAs are most effectively reduced by which interventions. The suggestion there's a lack of "skilled therapists used to working with intelligent, introspective clients" is a significant novel consideration for me as an aspiring psychologist and this kind of hybrid research could help me calibrate my intuitions.
Thanks for this! If you do this again, I'd love to see a comparison of mental health issues/experiences between a random sample of EAs, members of the public and members of other social movements.
Thanks for this!
Would it be possible for you to provide information on the quantity/frequency of the following findings?
1. "People find it difficult to find therapists who accept the values of Effective Altruism or whom they can trust"
2. "Thoughts on whether an EA-aligned therapist is necessary: some say yes, others no; some say it’s helpful to speak with therapists who are outside of the EA community."
Also, for 2, I'm curious whether they made claims about whether it was necessary or whether it was optimal. Seems quite different and my experience tells me that some growth areas (e.g., career-related beliefs and struggles) would be optimal for having someone EA-aligned (or at least EA-informed) whereas others wouldn't matter (e.g., ADHD).
Hi Sebastian! Sure thing! For both findings, they were findings that were not explicitly measured, but rather were provided as additional information by respondents, so please note that this is the case. That said:
I agree, from experience speaking with a few people, coaching with people who understand EA-values (though who do not necessarily identify with Effective Altruism themselves) is more helpful for some career-related growth areas, whereas support from medical and other mental health professionals who are willing to listen and try to understand (though who do not necessarily know much about Effective Altruism) seems to be ok for medical diagnoses and therapy.
Thanks so much for this reply - very informative.
This seems relatively aligned with my perspective although the specifics of what the therapists said in relation the strong moral values matter as moral perfectionism can be self-defeating. I'd also add that it seems as if older EAs are less concerned with EA-informedness than younger. For an example of why it might be beneficial to have an EA-informed coach or therapist, I quite liked this podcast episode on 80K.
Need help managing your own mental health and well-being? Check out the EA Mental Health Navigator!