Maternal Health Initiative (MHI) was founded out of Charity Entrepreneurship (AIM)’s 2022 Incubation Program and has since piloted two interventions integrating postpartum (post-birth) contraceptive counselling into routine care appointments in Ghana. We concluded this pilot work in December 2023.
A stronger understanding of the context and impact of postpartum family planning work, on the back of our pilot results, has led us to conclude that our intervention is not among the most cost-effective interventions available. We’ve therefore decided to shut down and redirect our funding to other organisations.
This article summarises MHI’s work, our assessment of the value of postpartum family planning programming, and our decision to shut down MHI as an organisation in light of our results. We also share some lessons learned. An in-depth report expanding on the same themes is available on our website.
We encourage you to skip to the sections that are of greatest interest:
- For people interested in the practicalities of development work, we recommend ‘MHI: An Overview of Our Work’.
- For those interested in family planning programming, we recommend ‘Pilot: Results’, ‘Why We No Longer Believe Postpartum Family Planning Is Among The Most Cost-Effective Interventions’, and ‘Broader Thoughts on Family Planning’.
- Finally, for those interested in broader lessons around entrepreneurship and organisation-building, we recommend ‘Choosing to Shut Down’ and ‘Lessons’.
Why we chose to pursue postpartum family planning
Why family planning?
Pregnancy-related health outcomes are a leading cause of preventable death among both mothers and children. In 2017, almost 300,000 women and girls died due to either pregnancy or childbirth (WHO, 2017). Cleland et al. (2006) estimate that comprehensive access to contraception could avert more than 30% of maternal deaths and 10% of child mortality globally.
Contraceptive access provides a wide range of other potential benefits, the most significant of which may be increasing reproductive autonomy for women who want to space or limit births and currently have limited options for doing so.
Why postpartum (post-birth)?
Postpartum family planning (PPFP) – that is, integrating family planning guidance into postnatal care and/or child immunisation appointments– has been identified as an effective way of increasing contraceptive uptake and reducing unmet need (Wayessa et al. (2020); Saeed et al. (2008); Tran et al. (2020); Tran et al. (2019); Pearson et al. (2020); Dulli et al. (2016).
The maternal and infant mortality risks from short birth spacing make the postpartum period a potential point of particular value from increased contraceptive access. Demographic Health Survey (DHS) analysis suggests an 18% increase in neonatal mortality, 21% increase in child mortality, and 32% increase in mortality risk from births that occur within two years of a prior pregnancy (Kozuki and Walker’s 2013; Conde-Agudelo et al. 2007).
While it is often an official policy that family planning counselling should be included in postnatal care (Ghana Health Service, 2014), the consistency and quality of family planning services in the postpartum period vary in practice (Morhe et al. 2017).
MHI: An overview of our work
Charity Entrepreneurship (AIM) recommended postpartum family planning as part of the 2022 Incubation Program through which MHI was founded. As such, MHI has had an explicit focus on postpartum family planning work since its beginning. We spent our first few months interviewing a few dozen experts, getting up to speed with research in the field, and selecting priority target countries. Based on this work, we visited Sierra Leone and Ghana in January and February 2023.
We struggled to find a viable partner organisation in Sierra Leone and our initial meeting with the national government there suggested lower enthusiasm for the kind of work we were proposing. However, our time in Ghana was more promising and we chose to launch pilot work in Northern Ghana with two local organisations - Norsaac and Savana Signatures.
Once our partnerships were in place, we began conducting baseline surveys and interviews with both healthcare providers and recipients to better understand family planning services and barriers to access in Ghana.
Building on this information, we ran an initial proof of concept training sessions in April 2023 with around 25 nurses and midwives. One-month follow-up surveying suggested that while providers had a strong knowledge of family planning post-training, implementation of counselling was inconsistent.
This information led us to redesign our intervention approaches in the summer of 2023, shifting from training providers on family planning knowledge and counselling best practices to training them in one of two specific, structured counselling models.
Through the second half of 2023, MHI’s efforts focused on refining and then evaluating these two models. We began by conducting a second proof of concept project with Savana Signatures at six hospitals in the Northern and Savannah Regions to test and refine the new intervention models. With this knowledge, we then launched a formal pilot project from September to December 2023 across six hospitals in Ghana’s Northern Region. Since its conclusion, MHI has focused on data analysis and investigation of the uncertainties around impact that have ultimately led us to the choice to shut down.

Pilot: Design
MHI’s pilot programme was based on two specific intervention models, with counselling materials designed by MHI to support providers in implementing this counselling. These models were the following:
Postnatal Care (PNC)
- Include family planning counselling as part of every 1:1 postnatal appointment
- Use MHI’s Counselling Guide as a framework for this discussion, with the Method Cards and Method Information Booklet used as key resources in this framework. The discussion should take around 20 minutes, depending on the number of questions from the client.
- Offer a method directly, or a referral to the family planning unit, for women who express an interest in taking up a method of birth spacing at the end of the counselling discussion.
Child Welfare Clinic (CWC)
- Include family planning messaging in every group talk given while women wait for their child to be called up for weighing and immunisation, using MHI’s streamlined ‘Birth Spacing Group Talk’ flipchart as a guide.
- Providers giving immunisations have a very short 1:1 family planning discussion with each woman as her child is vaccinated using the ‘Birth Spacing Card’.
- Offer women the option of a streamlined referral for family planning at the end of this one-to-one engagement, using a system of referral cards to make it simple for women to receive a method that day should they choose to do so.
These models were each selected to replicate a particularly promising RCT that we hoped would translate well to Northern Ghana. A study by Asah-Opoku et al (2023) in Accra concluded that one-to-one counselling as part of routine postnatal care sessions (PNC) was associated with a significantly greater uptake of contraception during the postpartum period. Meanwhile, Dulli et al (2016) found that incorporating family planning services into routine child welfare clinic sessions as part of immunisation provision resulted in a 15% shift in postpartum contraceptive use.
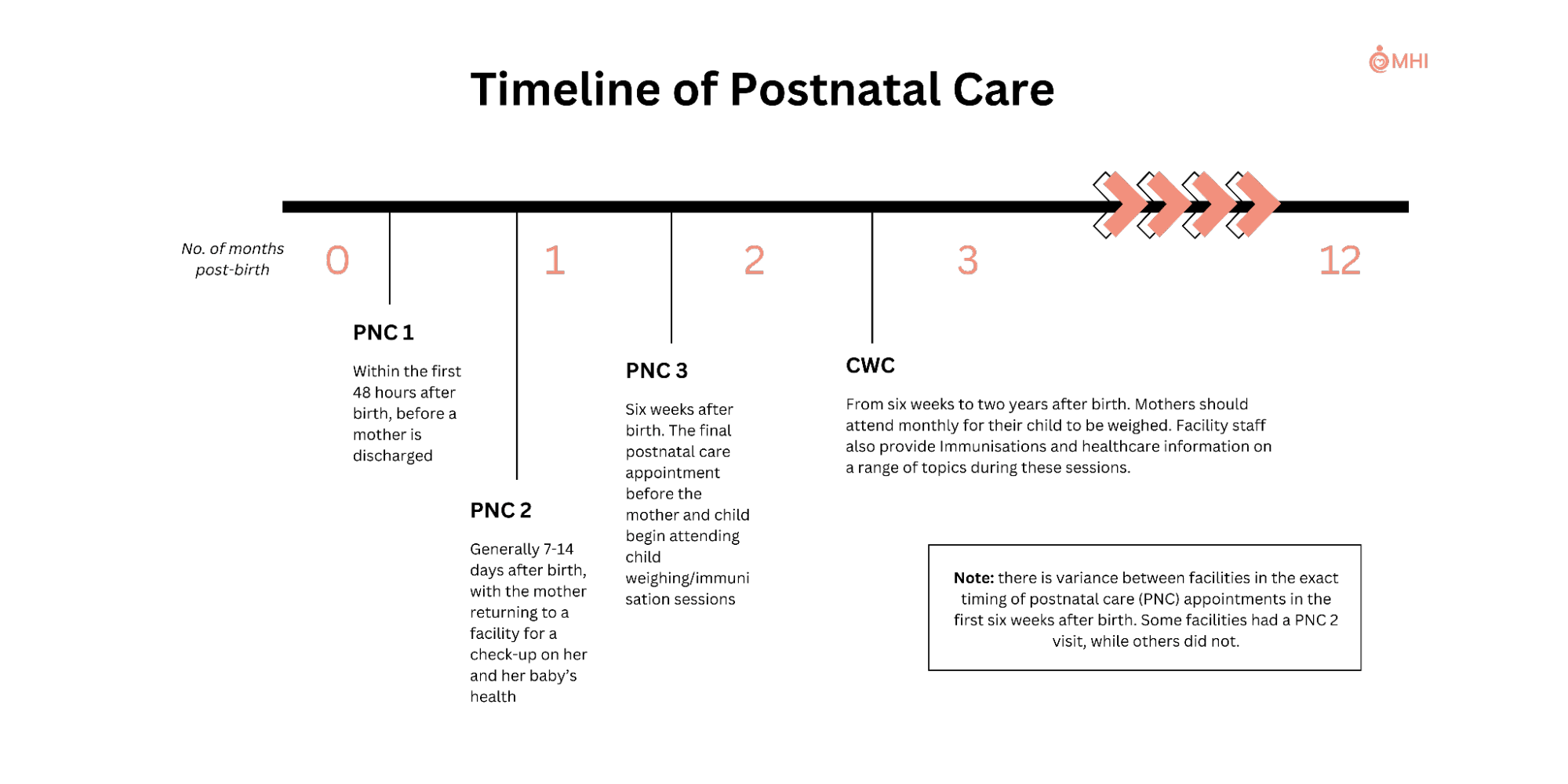
The two models targeted different points on the continuum of care after birth, with mothers attending up to three postnatal care (PNC) sessions from 0-6 weeks post-birth, and then attending child welfare clinics (CWC) sessions monthly from 6 weeks onwards.
A more detailed explanation and discussion of our pilot design is available in the project report on our website.
Pilot: Results
Sample Population
Our pilot surveyed women attending a PNC or CWC session at one of our target facilities. We surveyed 205 women pre-intervention, and 226 women six weeks after the training sessions.
The pre- and post-intervention groups were similar within the PNC and CWC intervention arms. Most respondents were Muslim, currently married, and had an average age of 27-28. The majority had previously used modern contraception and were currently abstinent, while almost all were currently breastfeeding.
Implementation
Our surveying results suggest that the implementation of family planning counselling increased significantly, with an increase of more than 20% seen across both interventions. However, this still fell short of the counselling consistency we had aimed for and likely diminished the pilot’s impact.
Variation between facilities suggests that substantially higher rates of counselling consistency are possible. Challenges in achieving these levels consistently were unsurprising given implementation issues in previous facility-based family planning programs (Pearson et al. 2020; Vance et al. 2013).
Table: Implementation Consistency
| PNC | CWC | |||||||
Baseline (n= 100) | Endline (n=106) | Difference | Baseline (n= 105) | Endline (n=120) | Difference | |||
| 1:1 Family Planning Counseling | Overall | 18.0% | 39.6% | 21.60% | Overall | 28.10% | 55.80% | 27.70% |
| Group Talk on Family Planning | N/A | Overall | 15.20% | 72.50% | 57.30% | |||
Changes in Contraceptive Uptake
No statistically significant effects on actual or intended contraceptive use in either arm were observed at immediate surveying. At the recommendation of local stakeholders, we also conducted 2-week follow-up surveying by phone to capture uptake that occurs after women consult with their husbands or other family members.
Data from a 2-week phone follow-up survey suggests a 22% increase in contraceptive use (p < .01) and a 25.3% increase in intended use (p = .0187) in the PNC arm and no statistically significant effects in the CWC arm. However, we have concerns about the robustness of this data given the reduced sample size and possible biases in this smaller sample.
Table: Changes in Contraceptive Use
| PNC | CWC | |||||||
| Baseline | Endline | Difference | p value | Baseline | Endline | Difference | p value | |
| Immediate Surveying | n=100 | n=106 | n=105 | n=120 | ||||
| Use of modern contraception (all facilities) | 2.00% | 5.00% | 3.00% | 0.446 | 15.20% | 14.20% | -1.00% | 0.821 |
| 2-week phone follow-up | (n= 50) | (n=41) | (n= 52) | (n=59) | ||||
| Use of modern contraception (all facilities) | 0% | 22.00% | 22.00% | 0.000447** | 15.40% | 13.60% | -1.80% | 0.794☨ |
Conclusions From Our Pilot Results
Based on a provisional cost-effectiveness analysis, we were aiming for a shift in contraceptive uptake of around 10% from our pilot program. Neither of MHI’s pilot interventions approached this level based on the immediate surveying. The 2-week follow-up data for PNC suggests a much larger shift in contraceptive uptake, though we have concerns about the reliability of this data.
Put together, these results suggest a few conclusions. First, we can say with relative confidence that the CWC intervention did not work as hoped. Implementation was poorer but sufficient to expect reliable results, and we found no meaningful change in contraceptive uptake. Second, we can conclude that the effectiveness of the PNC intervention is hard to determine. We have conflicting surveying data, suggesting both a relative failure to produce change and potentially highly significant shifts in contraceptive uptake. Altogether, this data suggests that the PNC intervention likely produced a more meaningful shift in contraceptive uptake, possibly approaching or exceeding the 10% threshold we had set out when starting the pilot.
As such, our decision to shut down is based primarily on further research we conducted in response to some of the findings of our pilot, rather than the efficacy of the pilot programming. We now believe that a 10% shift in postpartum contraceptive uptake is likely to still fall substantially below the cost-effectiveness threshold at which a program like this would be worth scaling. Postpartum family planning programmes appear to produce limited or no changes in pregnancy rates - due in large part to the prevalence of postpartum insusceptibility - meaning that we believe contraceptive uptake in this period may produce little improvement to health or autonomy. These conclusions are discussed in-depth in the following section.
Further information on our pilot results will be available in a forthcoming journal article.
Why We No Longer Believe Postpartum Family Planning Is Among The Most Cost-Effective Interventions
There are several important reasons why we no longer believe postpartum family planning programming is the best use of MHI’s resources. As these conclusions are based on substantial further research, some of this section is comparatively technical.
Evidence of Limited Effects on Unintended Pregnancies
Family planning interventions are typically assessed based on their effects on contraceptive uptake, under the assumption that increases in uptake will necessarily translate into reduced unintended pregnancies. Postpartum family planning has been recognized as a “proven” high-impact practice in family planning – and hence received significant funding – on that basis (HIP Partnership, 2022). However, our experience working in this space has led us to believe that the connection between contraceptive uptake and unintended pregnancies is less clear-cut.
Measuring the effects of family planning interventions on unintended and short-spaced pregnancies has not been prioritised; hence, the evidence is limited. However, the evidence available is not promising for the efficacy of postpartum programming. Of the three studies we found that measure the effects of facility-based postpartum family planning programming on pregnancy rates, two found no effect (Rohr et al. 2024; Coulibaly et al. 2021), and one found only a 0.7% decrease in short-spaced pregnancies (Guo et al. 2022). This suggests that facility-based programs may have limited to no effect on reducing unintended pregnancies despite increasing contraceptive uptake. More research investigating this area is needed to draw confident conclusions, but this is certainly concerning.
Increases in family planning uptake are primarily valuable insofar as they allow women to avert mistimed or unintended pregnancies. If modern contraceptive uptake does not change the likelihood of pregnancy, it will not have an impact on the rates of short-spaced pregnancies, maternal mortality, or other health outcomes. It will also do little to provide women with additional autonomy or control over their reproductive lives.
Surprisingly – or unsurprisingly, depending on your perspective – these studies do not appear to have generated much discussion regarding the usefulness of postpartum family planning programming itself. Even within the studies themselves, the results regarding pregnancy rates are not treated as particularly significant; in one study, for example, they are reported in a single line and receive no discussion (Coulibaly et al. 2021). However, we believe that they are very significant for evaluating the true impact of such programs and the lack of engagement speaks to the ease with which programs can focus on proxy rather than true endline measures of impact.
The Prevalence and Impact of Postpartum Insusceptibility
Postpartum insusceptibility describes the period after birth in which a mother is naturally at zero or extremely low risk of pregnancy due to a combination of sexual abstinence and amenorrhea due to breastfeeding.
Our study found very high rates of abstinence - 96% at baseline and 98.1% at endline in the PNC arm and 67.6% at baseline and 81.7% at endline in the CWC arm - coupled with near-universal breastfeeding practice. New users of contraception who are already protected by abstinence and/or breastfeeding will not incur additional benefits from modern forms of contraception. Investigating this further, we found that these results generalise across much of Sub-Saharan Africa. DHS data suggests the mean duration of postpartum insusceptibility is 14.57 months across 39 countries with available data.
Short-Spaced Pregnancies
We now believe that the impact of postpartum family planning programs in reducing short-spaced pregnancies is likely to be overstated - though again, more research into this would be beneficial.
Short-spaced births are associated with lower levels of education and income (Rutstein 2011). Poorer and less educated women are typically less likely to obtain maternal and newborn care at health facilities and less likely to use contraception (Doctor et al. 2018; Ba et al. 2019). This likely means programming like MHI’s affects a significantly lower proportion of short-spaced pregnancies than we first believed.
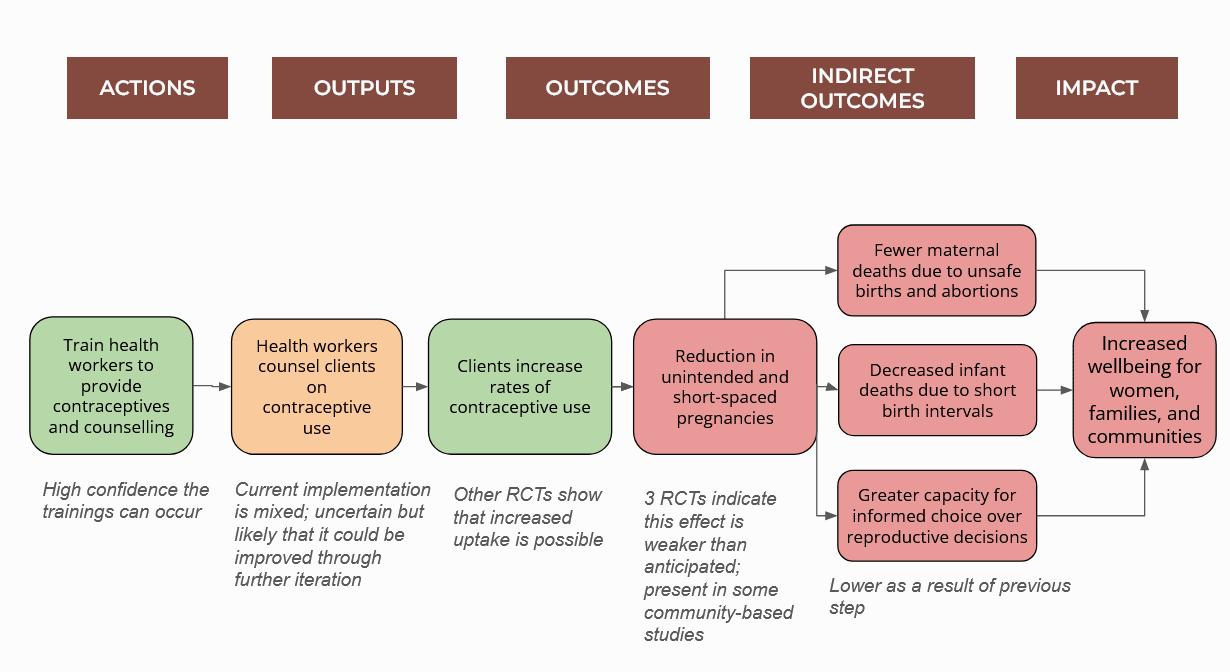
Theory of Change
Many of the above points feed into a revised assessment of the theory of change for postpartum family planning. This change is shown in the figure below, depicting our revised models for family planning’s theory of change and level of confidence in each stage of the causal chain.
Other Factors
Significant further concerns around discontinuation rates, cultural barriers, measurement of unmet need, and LARC-focused programming are discussed in our full report.
Broader Thoughts on Family Planning
The discussion above is focused on postpartum family planning programming specifically. However, there are both positive and negative conclusions on the value of family planning work more broadly that are worthy of discussion.
Concerns
Fertility Rate Change
This is an area of significant uncertainty but we believe more research is needed to demonstrate the robustness of the relationship between postpartum family planning uptake and fertility rate change. We expect that there is significant variation in the extent to which different types of family planning interventions drive reductions in unintended and short-spaced pregnancies. While our review of studies assessing facility-based postpartum family planning programs showed no strong effects on pregnancy rates (Rohr et al. 2024; Coulibaly et al. 2021; Guo et al. 2022), there is limited evidence of more promising results for other types of programs (Glennerster et al. 2022). Overall, there is a lack of robust evidence for such a crucial part of the theory of change for family planning work.
Side Effects
Robust and well-considered opposition to contraceptive use due to concerns around side effects is too frequently grouped together with wilder ‘myths and misconceptions’ as information barriers needing to be solved. Side effects like inconsistent or excess bleeding may be seen as relatively manageable in Western countries with more accepting cultural norms and practices but can be far more significant in low-income countries (Kulhmann et al., 2017; Polis et al., 2018).
Cultural practices around inconsistent or excess bleeding can prevent women from participating in a range of regular activities, including prayer, sexual activities, and community engagement (Bradley et al., 2009; Mohammed et al., 2020). Meanwhile, amenorrhea from contraceptive use is frequently interpreted as a sign of pregnancy and therefore potential promiscuity (Mackenzie et al. 2020). Given these consequences, the choice of some women not to use hormonal contraception in order to avoid these consequences is worthy of respect and support.
Reasons We Still Believe In The Importance Of Family Planning Work
Despite the points above, we still believe that some family planning interventions can be hugely impactful.
The need for action
Without aid investments in family planning, millions of women may be denied the opportunity to control whether and when to have children. Cultural barriers to family planning uptake that mean many women lack control over their reproductive lives may make cost-effective programming difficult but are not an excuse for inaction. Instead, they suggest the need for different approaches that more directly address and engage these cultural barriers rather than seeking to circumvent them.
Promising approaches
Mass media family planning interventions have the potential to reach millions of women at a greatly reduced cost compared to facility-based work. They also benefit from reaching the community as a whole, thereby addressing cultural barriers and encouraging discussion amongst couples that may lead to changes in desired family size.
We are also enthusiastic about more family planning interventions focused on supply rather than demand. Stockouts of contraceptive methods - when a facility has no supply of a commodity on a given day - prevent women who already wish to use family planning from taking up a method. Supply chain management interventions show promise in reducing stockouts (Krug et al. 2020), albeit with a shallow basis of evidence.
Autonomy
Finally, and perhaps most importantly, family planning programming is worthwhile for its effects on women’s autonomy. There are few decisions that are likely to be more significant in a person’s life than whether and when to have children. Measuring improvements to autonomy is difficult, even more so when trying to compare potential interventions. With that said, we believe that providing family planning information and access to women with genuine unmet need is likely to be one of the most impactful ways of increasing autonomy. Given people will often sacrifice a significant degree of wealth, happiness, and health for a greater degree of freedom, increasing autonomy may be one of the most significant avenues for improving people’s lives.
Choosing to Shut Down
There are uncertainties and caveats to all broader research conclusions. Our assessment of the value of postpartum family planning is far from immune to these. With that said, the analysis and reasoning summarised above give us a strong sense that postpartum family planning is unlikely to be as cost-effective as other approaches to increasing family planning access, and other approaches in global health more broadly.
MHI was founded with an explicit goal of starting one of the most effective charities in the world. If a new organisation such as ours does not exceed the value of existing work, we are merely shifting impact rather than creating additional value. As such, our conclusions around the lowered value of postpartum family planning left us with a choice to either pivot or shut down.
Considering a Pivot
A pivot makes sense when an organisation has clear comparative advantages that it can leverage into a new area of work. For MHI, we believe our primary comparative advantages were significant experience and stakeholder relationships in delivering healthcare facility-based interventions in Ghana and substantial experience and knowledge in delivering family planning programming.
Ultimately, we decided that a pivot in either of these directions did not seem sufficiently compelling to be worth pursuing.
Why not pivot to a different area of work in Ghana?
We chose to work in Ghana because of its rates of unmet need, strong healthcare system, and relatively low contraceptive uptake. We now believe that Ghana is unlikely to be one of the most cost-effective countries to work in for the majority of interventions. Our aim was to pilot a system of integrating contraceptive counselling into routine care that could be adopted by a national healthcare system. This long-term vision of government adoption meant that a more resilient and centrally managed healthcare system such as Ghana’s may prove more cost-effective than a country with higher baseline need.
We believe that this was a worthwhile approach, albeit one that did not work out in hindsight. However, the choice to work in Ghana means that MHI built stakeholder relationships and operating expertise in a country with relatively better healthcare outcomes across most indicators compared to other countries in sub-Saharan Africa.
This means that other work MHI could have pivoted to in Ghana was unlikely to be as cost-effective as a new project or other similar organisations working in different countries with higher burdens of disease and mortality.
Why not pivot to another family planning intervention?
We believe that there are other approaches to increasing contraceptive uptake that are likely to be effective in producing positive outcomes. There are several other family planning interventions we believe may be highly promising: mass media for social behaviour change, the direct provision of contraceptive methods, reductions in facility-level contraceptive stockouts, and policy shifts in who can offer methods and how methods are procured.
However, there is a wealth of both large and small organisations - such as Clinton Health Access Initiative (CHAI), Jhpiego, MSI, Lafiya Nigeria and Family Empowerment Media - that are already delivering family planning work that appears to be producing significant impact. This reduces the counterfactual of pivoting MHI to another family planning approach.
More significantly, there is a difficult question of personal enthusiasm and belief in an area of work. For one of us, family planning is no longer an intervention area that we want to work in due to some of the critiques raised in the ‘Broader concerns with family planning’ section. Elements of these critiques are an area of respectful disagreement between co-founders. However, given neither co-founder wanted to pursue an MHI pivot on their own, it significantly undermines any case for MHI to pivot into a different area of family planning work.
Proceeding to Shut Down
The value of pivoting an existing organisation, in comparison to starting a new one, is hard to determine. However, we believe that the value of MHI at this stage in its development lies predominantly in the knowledge and skills of the people involved.
By shutting down and potentially starting something new, our skills can be used on the most useful things rather than what makes the most sense within the scope of MHI. Similarly, by shutting down we can redirect MHI’s funding to other organisations with more promising signs of success. Founding is also demanding work - time away is likely to make us both more effective at whatever project we contribute to next. While pivoting MHI would have some benefits, we think these are significantly outweighed by the benefits of stepping away laid out above.
Lessons
While we think MHI’s programming was ultimately undermined by the reduced value of postpartum family planning compared to other interventions, there are more than enough mistakes that we made that may have improved the quality of our intervention. In the hope that other organisations may benefit from these lessons, we have explored some of them below.
Insufficient clarity of focus
As founders and directors of MHI, we were ambitious in what we set out to achieve.
While this was admirable, with hindsight it is clear that we attempted to deliver far too many things simultaneously. In choosing to do a lot of different things, we undermined our ability to do the few, most important things exceptionally well. There was a mismatch between our desire for speed and our willingness to streamline things. Choosing to test one intervention arm rather than two in our pilot would have allowed us to focus far greater resources on refining its design and implementation. Too much time spent on organisation-building (communications; internal process improvements; funder relationships) detracted from the time available for improving our programming: the core driver of whether or not MHI would be successful.
Developing a program offers a seemingly infinite number of avenues of work that appear worthwhile. Many things seem likely to make your program better. However, the choice to pursue an additional research question, monitoring strategy, or surveying metric is almost never a choice to do one more thing. It is a choice to do one more category of things, and will likely produce many more questions and areas of work needing to be completed in the process of solving a singular question or issue. In this way, each additional avenue of work that you pursue increases the burden of work exponentially.
The solution to this is a clear vision of your organisation’s priorities and perhaps a willingness to cut and discard more areas of work than seems reasonable. If you are only choosing not to do things that feel superfluous, you are likely not streamlining your work nearly enough.
Consistent underconfidence as an organisation
It is easy - and to some extent entirely justified - to feel imposter syndrome when founding an organisation in a field in which neither co-founder has prior experience. While this makes sense, MHI likely suffered from a collective underconfidence.
In our approach to working in Ghana, we positioned ourselves as a small actor with much to learn. In our first meetings with key stakeholders, we had a lot of open questions, lacked a clear vision of what kind of program we wanted to implement, and were reluctant to push for demanding requests or requirements. While this was very reasonable, it also spoke to an excess level of underconfidence that undermined MHI’s work. Asking for more from the government and from our partners may have felt a little unreasonable given our lack of experience, but would have made elements of our work significantly easier.
More broadly, it is easy to worry too much about external signals of what a successful organisation should do or look like. Are we getting to the point of running a pilot swiftly enough? Is this the stage at which we should begin hiring staff? How much research do other organisations do before committing to a country of operation? These are the wrong type of questions to ask. What matters is how these decisions make sense in the context of your organisation and your program. When do you need pilot results to be able to raise further funding before your seed funding runs out? What benefits would a new staff member bring relative to the costs of hiring and management time? What are the key questions we need to answer to know which country is most promising to start work in and how do we answer these?
While we likely believed at the time that our decisions were based on questions specific to our organisation, with hindsight some of these key decisions seem overly swayed by considerations about what people would expect an organisation like ours to be doing in this circumstance.

Data Collection Challenges
Throughout our work, we grappled with the difficulty of acquiring reliable data about confidential counselling through a public healthcare system. We had hoped to use facility-level data to assess how MHI’s programming affected the long-term trends in contraceptive uptake. Sadly, facilities had frequent gaps in their records and some records appeared to be duplicates, leaving little scope to trust the reliability of the facility-level data we received.
The quality of the surveying delivered through our partner organisations was significantly higher. However, we struggled to find mechanisms for collecting data free from potential bias. In one case, our client and provider surveying data suggested MHI’s materials were in use for counselling during a CWC session that we attended in person, yet our own observation highlighted that they were not.
Our best, though imperfect, solution to this was to triangulate data from multiple sources in order to determine the reliability of each source. The CWC session above is a good example of this in practice, with in-person observation allowing us to assess the reliability of observation from our partners, client surveying data, and provider surveying data.
Willingness to spend
In part due to our data collection issues, we spent a significant amount of time debating and investigating uncertainties around our program through desk research that could have been resolved far more swiftly through fieldwork. Knowing your organisation’s weekly or monthly burn rate - the amount it costs just to keep the lights on each month - can encourage spending on the most useful things. Additional monitoring work may seem prohibitively expensive at a cost of $5,000, but it pays for itself if it saves more than two weeks of work for an organisation with 2+ staff by resolving the causes of implementation issues.
Conclusions
Shutting down MHI was not the outcome we wished for when we founded the organisation in the summer of 2022. While our pilot likely failed to deliver the impact we had hoped, we believe with further iteration and improved implementation the impact on contraceptive uptake likely would have increased. Ultimately, this decision is based on concerns around the endline impact of our programming: changes in maternal and child health, and maternal autonomy. Rates of postpartum insusceptibility and method discontinuation, reduced impact on short-spaced pregnancies, incorrect estimates of unmet need, weak data connecting uptake to pregnancy rate shifts, and the importance of cultural barriers to uptake combine to suggest that postpartum family planning is unlikely to be as cost-effective as the top alternative family planning and global health interventions.
Upon drawing these conclusions, we considered pivots to other facility-based interventions in Ghana or other areas of family planning work in other countries. However, we believe that a pivot in these directions is unlikely to be the best use of MHI’s resources relative to redirecting the talent and funding to other new or existing organisations. This left us with the decision to shut down MHI’s operations.
It is essential that organisations are willing to hold themselves to high standards and shut down if they do not believe their work is effective. The value of new development charities - such as those set up by Charity Entrepreneurship (AIM) - is largely dependent on finding avenues for additional impact relative to existing organisations pursuing similar work. We set out with the aim of creating one of the most cost-effective charities in the world. In acknowledging our likely failure to reach this standard, we hope to encourage other organisations to engage deeply with the impact and counterfactuals of their own work with a willingness to shut down if this appears appropriate.
Thank you for taking the time to engage with MHI’s work and decision to shut down. There are countless lessons to learn from projects that do not succeed, perhaps as many or more as the lessons available from large successes. If you would like to learn more about our work or discuss the conclusions we have drawn from it, please visit our website or reach out to us directly through the contact details at the end of this report.
Acknowledgements
We would like to finish by saying thank you to the countless incredible people who have worked for, supported, and funded MHI since we began in 2022.
Thank you to Anthony Suguru Abako, Enoch Weikem Weyori, Abdul Rahman Issah and the rest of the Norsaac team for their resourcefulness and energy in delivering so much of our pilot work. Thank you to Emefa Ehla, Rahana Mohammed, Racheal Antwi, and the rest of the Savana Signatures team for their hard work and insight throughout the delivery of our proof-of-concept projects.
Thank you to our skilful facilitator, Sulemana Hikimatu Tibangtaba, for delivering high-quality and engaging training sessions. Thank you to Sofía Martínez Gálvez and Catherine Fist for their insights and endeavour as MHI staff helping to design and implement this project. Thank you to MHI’s many volunteers and interns who gave up their time and energy for free, particularly Jemima Jones, Wan Yun Tan, Maxine Wu and Samuel Harvey.
Thank you to everyone at Charity Entrepreneurship for setting us on this journey and helping us so much along the way.
Lastly, thank you to MHI’s donors and supporters, without whom this project would not have been possible.
We are indebted to you all for your generosity of effort, time, and money and incredibly grateful for your commitment to making the world a better place for all.

Thanks for putting this post together. It takes fortitude to commit so much to an altruistic project, and it takes integrity to make this decision and write up this explanation.
Thank you for trying <3
Thank you for your integrity, and congratulations on your successful research into the cost-effectiveness of this intervention!
Strongly upvoted. Posts like this are painful to write, but really valuable to read. Thanks for putting it together
Disclosure: Sarah and Ben are friends, and we came out of the same CE incubation batch, so I'm not unbiased here.
I think it's speaks well of a person's integrity, objectivity, and concern for impact that they're able to make a clear eyed assessment that their own project isnt having the desired impact, and then going ahead to shut it down so as to not burn counterfactually valuable resources.
It's something that's worth emulating, and I do try to apply this myself - via regular CEAs and qualitative evaluations of CEAECH's expected impact (especially as a meta org with a more indirect path to impact). We're only wasting our own time otherwise!
I was surprised by the "Concerns" section being so short, and noticed that the pdf on the website goes into much more detail. I found the additional considerations there really interesting.
I only briefly skimmed it, but the whole report seems really interesting.[1] Thank you so much for working on it and sharing this!
E.g. how "unmet need" is a misleading metric
Good on you for being courageous and scout-minded enough to shut this down (and to start it in the first place)! I hope you find great projects to move onto.
Top notch work. My two favourite things about this community are 1) the willingness to take a serious crack at working on whatever project seems like it will help most people and 2) the integrity to shut down projects that do not meet expectations. Your work exemplifies both.
Great effort on the project, and appreciate the open sharing which helps everyone out 👏
Thanks for this detailed report. It's likely to be helpful to other organizations to understand the reasoning and evidence base behind this in considering whether to start or fund adjacent projects. Il
Some things that woukd also be nice com apologise if you already did this.
Can you share your data and code or spread sheets in case other researchers or founders want to revisit this? potentially this is something students and academic researchers would want to help you with.
You often report pre-values and a “lack of significant difference". Of course, this could be driven by lack of statistical power in small samples. it would be helpful if you could report, confidence intervals for these. if you have the bandwidth, it would be helpful if you could do some equivalent test or even Bayesian analysis in a decision framework.
We will be publishing a journal article with our pilot findings that goes into all of the data and has much more advanced statistical analysis -- we'll be sure to share that here as well! We're also planning to publish a commentary that focuses on our broader concerns on postpartum family planning and digs into that data. I totally agree that what we've shared here is just a small sliver of the data.
FYI: The link to the summary (https://maternalhealthinitiative.org/final-summary-of-our-work/) does not seem to work for me (404).
I ran into the same issue. It looks like the report is still live at this URL, though! (And here's an archived version)
This link should now be fixed!
Executive summary: Maternal Health Initiative (MHI) is shutting down after concluding that postpartum family planning interventions are not as cost-effective as initially believed, based on pilot results in Ghana and further research into the impact of such programs.
Key points:
This comment was auto-generated by the EA Forum Team. Feel free to point out issues with this summary by replying to the comment, and contact us if you have feedback.
Thanks for writing this! As others have said, thank you for trying to do this valuable work even if it didn't work out.
I haven't read everything so sorry if you mention this elsewhere but I'm confused about:
-'Of the three studies we found that measure the effects of facility-based postpartum family planning programming on pregnancy rates, two found no effect (Rohr et al. 2024; Coulibaly et al. 2021), and one found only a 0.7% decrease in short-spaced pregnancies (Guo et al. 2022).
This suggests that facility-based programs may have limited to no effect on reducing unintended pregnancies despite increasing contraceptive uptake.'
Why might programs increase contraceptive uptake but not reduce unintended pregnancies? Is it mainly because many who take the contraceptives are in the postpartum insusceptibility period anyway?
Thanks for the kind words! This is a great question. There's a lot of uncertainty here but here's a few thoughts:
Thanks for choosing an important topic (maternal health) which can greatly affect infant and whole family health and prosperity.
Historically, the interventions which lead to a very helpful 2 year gap between pregnancies are called "birth spacing" or just "spacing". If others are interested in this, or stunting, or impacts on educational attainment/IQ, a lot is available.
USAID's work on the BASICS programme and its successors is especially important, and produced a lot of effectiveness outputs and lessons learned, available now through me, in books, and via Scholar searches like this one on Ghana.
Some categories to bear in mind:
- for behaviour change in parental or sexual practices, single interventions of a limited duration are rarely effective; multiple tactics over an extended period work better; good examples include USAID BASICS approach to increasing breast-feeding and vaccination in Madagascar, using women's drama groups, radio, artists, flags on clinics, positive deviants, income-generation etc all in the same district
- a properly participatory approach (PLA) and (ideally) community-led approach is more likely to work and sustain itself; this takes more initial negotiation, and experienced community workers, but it pays off handsomely.
- this is an area where expertise and field experience in specific IRL context do matter: there are so many things to get wrong, and people have been working on effectiveness, health economics and RTCs for decades. This does not mean EAs have no role, but talking to larger NGOs/sector funders and asking them to identify gaps can be a good strategy. If an NGO repeatedly gets USAID, GIZ and French funding and has been around in a country for 20 years, they have probably achieved some good impacts and know some unmet needs and opportunities. NGOs are often friendly about networking and referals. (Try the Hash House Harriers or English-speaking church or embassy events, ot stop by at the Netherlands Embassy, often helpful and pragmatic)
I'm happy to be called about this, and any global health/poverty issues.
Thank you for sharing this incredible brief of your experience.